Clin Endosc.
2017 Sep;50(5):504-507. 10.5946/ce.2017.012.
Two Cases of Plug or Stone in Remnant Intrapancreatic Choledochal Cysts Treated with Endoscopic Retrograde Cholangiopancreatography
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University College of Medicine, Chungbuk, Korea. smpark@chungbuk.ac.kr
- 2Department of Radiology, Chungbuk National University College of Medicine, Chungbuk, Korea.
- 3Department of Surgery, Chungbuk National University College of Medicine, Chungbuk, Korea.
- KMID: 2394753
- DOI: http://doi.org/10.5946/ce.2017.012
Abstract
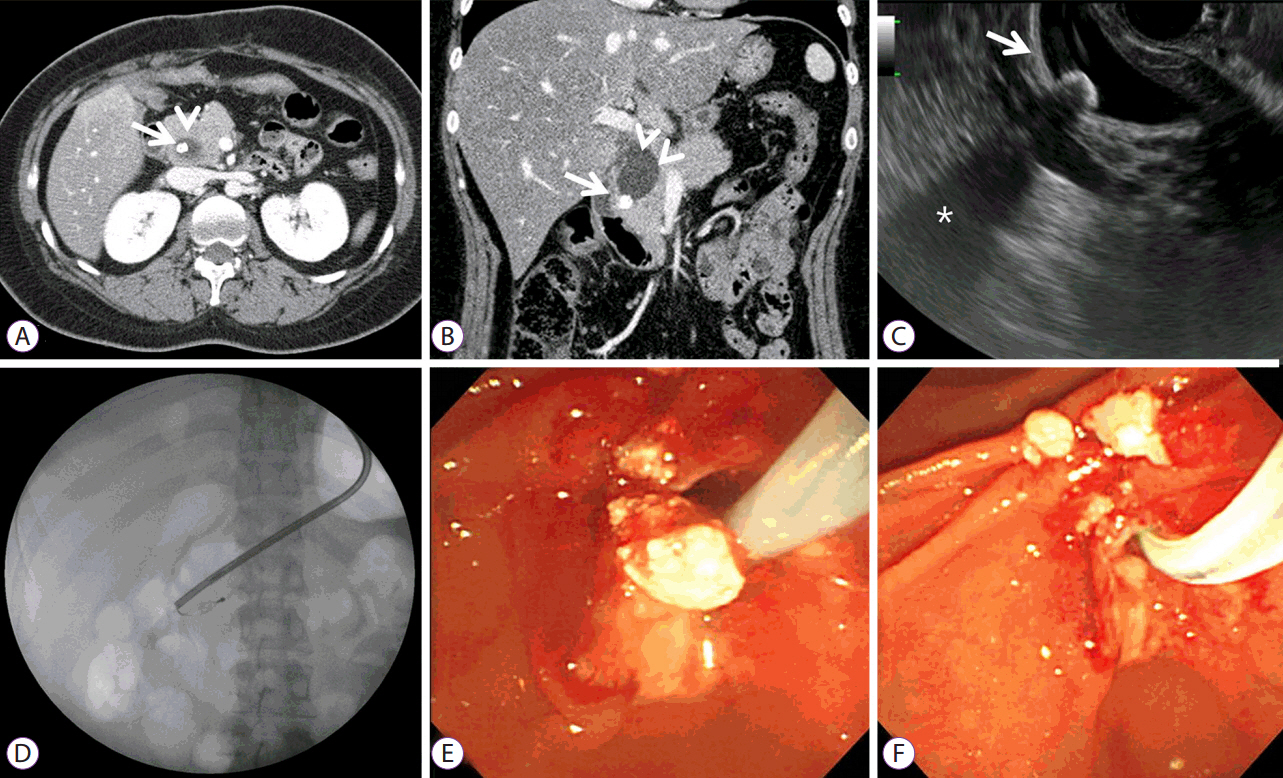
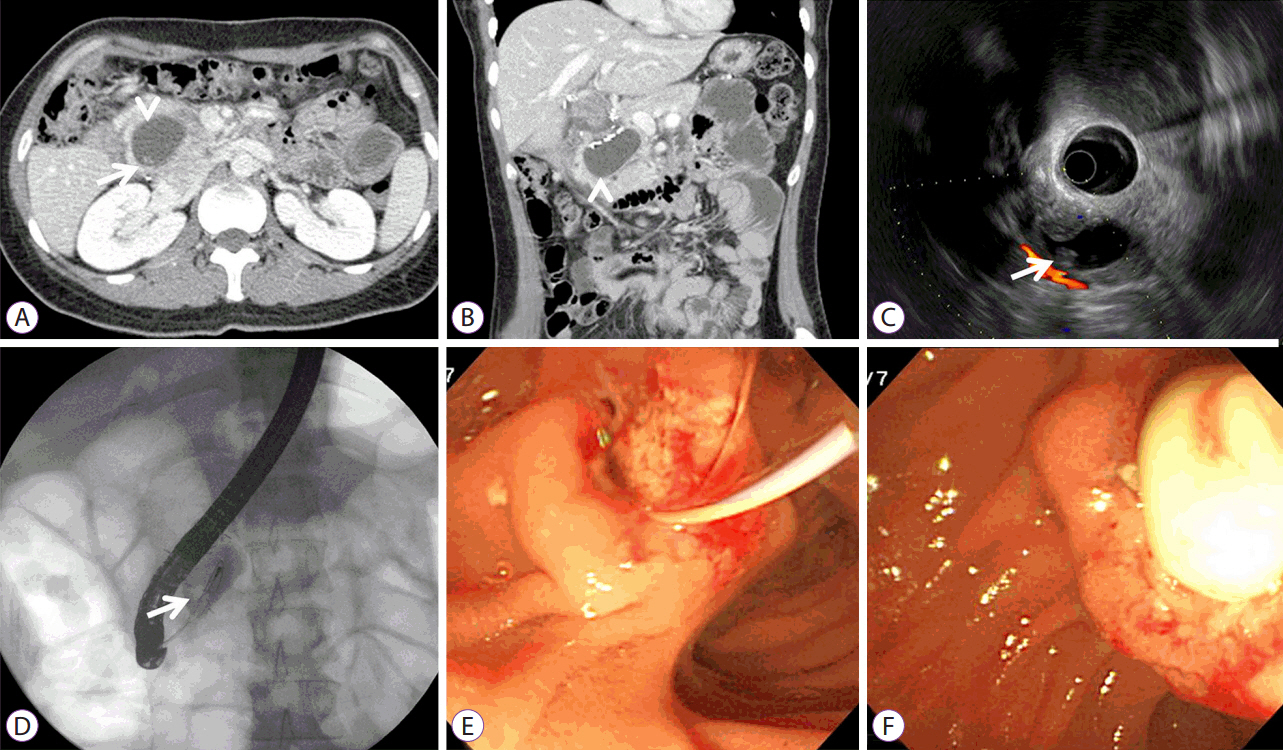
- Incomplete resection of choledochal cysts (CCs) that extend deep into the pancreas can lead to protein plug or stone formation, pancreatitis, and cholangiocarcinoma. We encountered two cases of choledocholithiasis in remnant intrapancreatic CCs, in which the patients exhibited symptoms after 3 and 21 years of cyst excision. A 21-year-old woman who had undergone excision of a CC, as a neonate, presented with epigastric pain. Abdominal computed tomography (CT) revealed stones inside the remnant pancreatic cyst, which were removed by endoscopic retrograde cholangiopancreatography (ERCP), and her symptoms improved. A 33-year-old woman, who underwent cyst excision 3 years ago, presented with pancreatitis. Abdominal CT showed a radiolucent plug inside the remnant pancreatic cyst. The soft, whitish plug was removed by ERCP, and the pancreatitis improved. These cases indicate that plugs and stones in CCs have the same pathogenetic mechanism, and their form depends on the time since the incomplete excision surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Todani T, Tabuchi K, Watanabe Y, Kobayashi T. Carcinoma arising in the wall of congenital bile duct cysts. Cancer. 1979; 44:1134–1141.
Article2. Cheung TT, Fan ST. Technical note on complete excision of choledochal cysts. Hepatobiliary Pancreat Dis Int. 2013; 12:218–221.
Article3. Kaneko K, Ando H, Ito T, et al. Protein plugs cause symptoms in patients with choledochal cysts. Am J Gastroenterol. 1997; 92:1018–1021.4. Chiba K, Kamisawa T, Egawa N. Relapsing acute pancreatitis caused by protein plugs in a remnant choledochal cyst. J Hepatobiliary Pancreat Sci. 2010; 17:729–730.
Article5. Jordan PH Jr, Goss JA Jr, Rosenberg WR, Woods KL. Some considerations for management of choledochal cysts. Am J Surg. 2004; 187:790–795.
Article6. Hsu RK, Yu A, Lee JG, Leung JW. Pancreatitis caused by common bile duct stones in a 3-year-old boy with prior surgery for a choledochal cyst. Am J Gastroenterol. 2001; 96:1919–1921.
Article7. Nakano K, Mizuta A, Oohashi S, et al. Protein stone formation in an intrapancreatic remnant cyst after resection of a choledochal cyst. Pancreas. 2003; 26:405–407.
Article8. Kim JW, Moon SH, Park DH, et al. Course of choledochal cysts according to the type of treatment. Scand J Gastroenterol. 2010; 45:739–745.
Article9. Takahashi T, Shimotakahara A, Okazaki T, et al. Intraoperative endoscopy during choledochal cyst excision: extended long-term follow-up compared with recent cases. J Pediatr Surg. 2010; 45:379–382.
Article10. Urushihara N, Fukumoto K, Fukuzawa H, et al. Long-term outcomes after excision of choledochal cysts in a single institution: operative procedures and late complications. J Pediatr Surg. 2012; 47:2169–2174.
Article11. Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012; 18:4801–4810.
Article12. Ohashi T, Wakai T, Kubota M, et al. Risk of subsequent biliary malignancy in patients undergoing cyst excision for congenital choledochal cysts. J Gastroenterol Hepatol. 2013; 28:243–247.
Article13. Xia HT, Yang T, Liang B, Zeng JP, Dong JH. Treatment and outcomes of adults with remnant intrapancreatic choledochal cysts. Surgery. 2016; 159:418–425.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Choledochocele containing a stone mistaken as a distal common bile duct stone
- A Clinical Analysis of Choledochal Cyst
- Development of Cholangiocarcinoma Arising from Remnant Intrapancreatic Cyst 15 Years after Choledochal Cyst Excision
- Clinical Significance of Anomalous Pancreaticobiliary Ductal Union Diagnosed by Endoscopic Retrograde Cholangiopancreatography
- A Case of Intrahepatic Choledochal Web That Was Diagnosed by Percutaneous Transhepatic Cholangioscopy and It Was Treated with Balloon Dilatation: Review of the Korean Cases