J Korean Soc Radiol.
2017 Nov;77(5):339-343. 10.3348/jksr.2017.77.5.339.
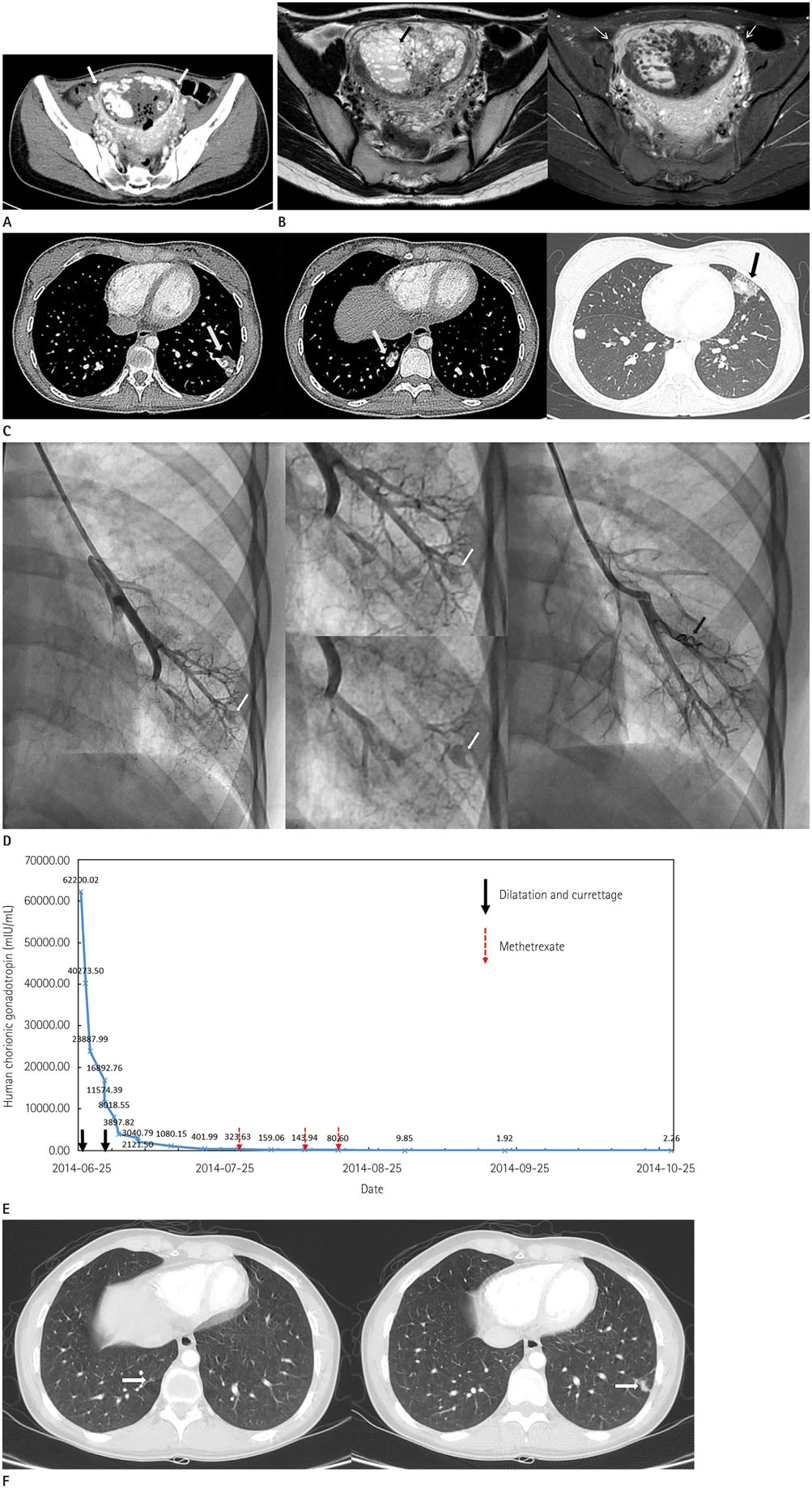
Accompanying Pulmonary Arteriovenous Malformation in Patient with Hydatidiform Mole: A Case Report
- Affiliations
-
- 1Department of Radiology, Kangwon National University Hospital, Chuncheon, Korea. hk2005.yoon@gmail.com
- 2Department of Obstetrics and Gynecology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Kangwon National University School of Medicine, Kangwon National University Hospital, Chuncheon, Korea.
- KMID: 2394049
- DOI: http://doi.org/10.3348/jksr.2017.77.5.339
Abstract
- The most common site of metastasis in gestational trophoblastic disease (GTD) is the lung. To the best of our knowledge, arteriovenous malformations (AVMs) associated with pulmonary metastatic lesions are extremely rare in patients with GTD. Here, we report a case of a nineteen-year-old woman who presented with pulmonary AVMs which developed in the areas of pulmonary metastases, complicated by recent hemorrhage.
MeSH Terms
Figure
Reference
-
1. Shanbhogue AK, Lalwani N, Menias CO. Gestational trophoblastic disease. Radiol Clin North Am. 2013; 51:1023–1034.2. McDonald-Burrows Z, Davies R, Goode E, Clarke C, Jackson J, Seckl M, et al. Haemoptysis from a pulmonary arteriovenous malformation in a post molar pregnancy gestational trophoblast tumour patient managed by radiological embolisation: a case report. J Med Case Rep. 2014; 8:117.3. McGrath S, Harding V, Lim AK, Burfitt N, Seckl MJ, Savage P. Embolization of uterine arteriovenous malformations in patients with gestational trophoblastic tumors: a review of patients at Charing Cross Hospital, 2000-2009. J Reprod Med. 2012; 57:319–324.4. Zygmunt M, Herr F, Münstedt K, Lang U, Liang OD. Angiogenesis and vasculogenesis in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2003; 110:Suppl 1. S10–S18.5. Touhami O, Gregoire J, Noel P, Trinh XB, Plante M. Uterine arteriovenous malformations following gestational trophoblastic neoplasia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2014; 181:54–59.6. Green JD, Carden TS Jr, Hammond CB, Johnsrude IS. Angiographic demonstration of arteriovenous shunts in pulmonary metastatic choriocarcinoma. Radiology. 1973; 108:67–70.7. Shovlin CL. Pulmonary arteriovenous malformations. Am J Respir Crit Care Med. 2014; 190:1217–1228.8. Pick A, Deschamps C, Stanson AW. Pulmonary arteriovenous fistula: presentation, diagnosis, and treatment. World J Surg. 1999; 23:1118–1122.9. Casson AG, McCormack D, Craig I, Inculet R, Levin L. A persistent pulmonary lesion following chemotherapy for metastatic choriocarcinoma. Chest. 1993; 103:269–270.10. Choi SH, Goo JM, Kim HC, Im JG. Pulmonary arteriovenous fistulas developed after chemotherapy of metastatic choriocarcinoma. AJR Am J Roentgenol. 2003; 181:1544–1546.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of Arteriovenous Malformation of the Uterus complicated with Hydatidiform Mole
- A case of trophoblastic pulmonary embolization associated with hydatidiform mole
- A Case of Ectopic Hydatidiform Mole in the Uterine Cornua
- A case of membranoproliferative glomerulonephritis associated with a hydatidiform mole
- A Case of Twin Pregnancy with a Complete Hydatidiform Mole and co-existing Fetus