J Korean Orthop Assoc.
2017 Oct;52(5):453-461. 10.4055/jkoa.2017.52.5.453.
Management of Melorheostosis
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonnam National University Medical School, Gwangju, Korea. stjung@chonnam.ac.kr
- KMID: 2393519
- DOI: http://doi.org/10.4055/jkoa.2017.52.5.453
Abstract
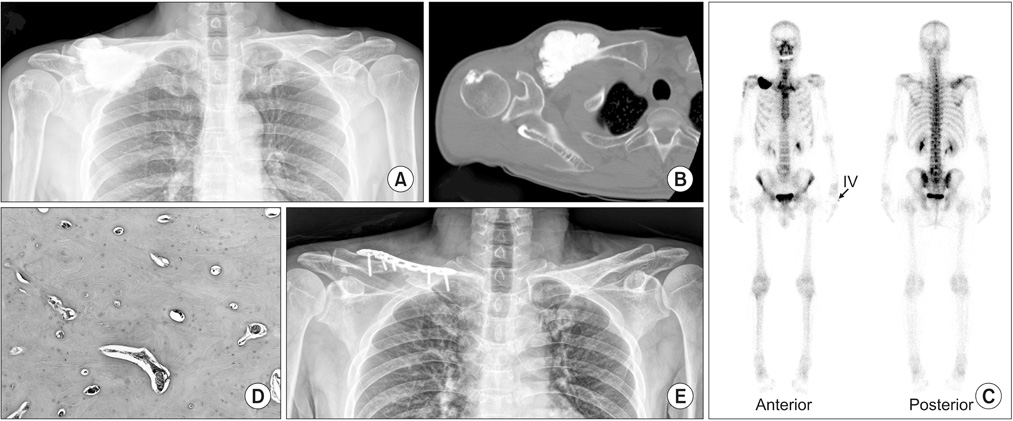
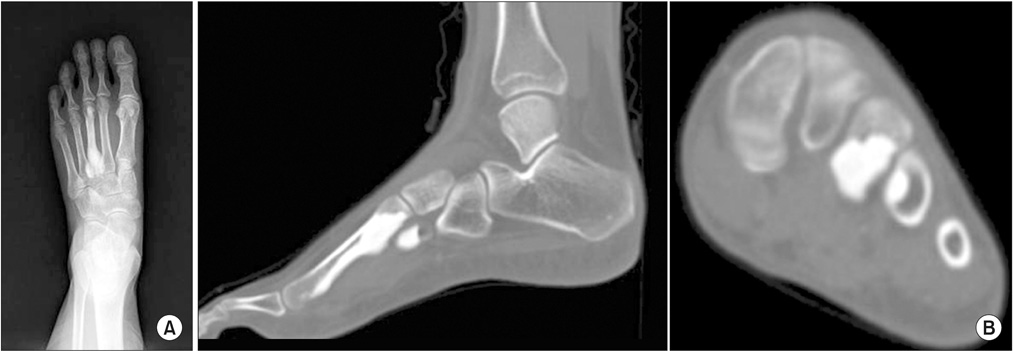
- Melorheostosis is a very rare sclerosing bone disease with pain, joint stiffness, and limitation of motion. Its characteristic on radiography is a dense bone formation along the side of the bone, resembling the flow of candle grease. Various conservative or surgical methods have been practiced in treating pain and deformities. This is a report on the successful treatment result of six cases of melotheostosis, involving the metatarsal, metacarpal, clavicle, and tibia, which weretreated by conservative and operative treatment methods.
Keyword
MeSH Terms
Figure
Reference
-
1. Gagliardi GG, Mahan KT. Melorheostosis: a literature review and case report with surgical considerations. J Foot Ankle Surg. 2010; 49:80–85.
Article2. Jain VK, Arya RK, Bharadwaj M, Kumar S. Melorheostosis: clinicopathological features, diagnosis, and management. Orthopedics. 2009; 32:512.
Article3. Leri A, Joanny J. Une affection non decrite des os: hyperostose ‘en coulee’ sur toute la longueur d' un membre ou ‘melorheostose’. Bull Mem Soc Med Hop Paris. 1922; 46:1141–1145.4. Campbell CJ, Papademetriou T, Bonfiglio M. Melorheostosis. A report of the clinical, roentgenographic, and pathological findings in fourteen cases. J Bone Joint Surg Am. 1968; 50:1281–1304.5. Freyschmidt J. Melorheostosis: a review of 23 cases. Eur Radiol. 2001; 11:474–479.
Article6. Younge D, Drummond D, Herring J, Cruess RL. Melorheostosis in children. Clinical features and natural history. J Bone Joint Surg Br. 1979; 61:415–418.
Article7. Jung ST, Jung SN, Lee KB. Melorheostosis of the foot. A case report. J Korean Orthop Assoc. 2000; 35:177–180.8. Greenspan A, Azouz EM. Bone dysplasia series. Melorheostosis: review and update. Can Assoc Radiol J. 1999; 50:324–330.9. Morris JM, Samilson RL, Corley CL. Melorheostosis. Review of the literature and report of an interesting case with a nineteen-year follow up. J Bone Joint Surg Am. 1963; 45:1191–1206.10. Slimani S, Nezzar A, Makhloufi H. Successful treatment of pain in melorheostosis with zoledronate, with improvement on bone scintigraphy. BMJ Case Rep. 2013; 2013. Published online June 21, 2013. DOI: 10.1136/bcr-2013-009820.
Article