Korean Circ J.
2017 Jul;47(4):425-431. 10.4070/kcj.2016.0237.
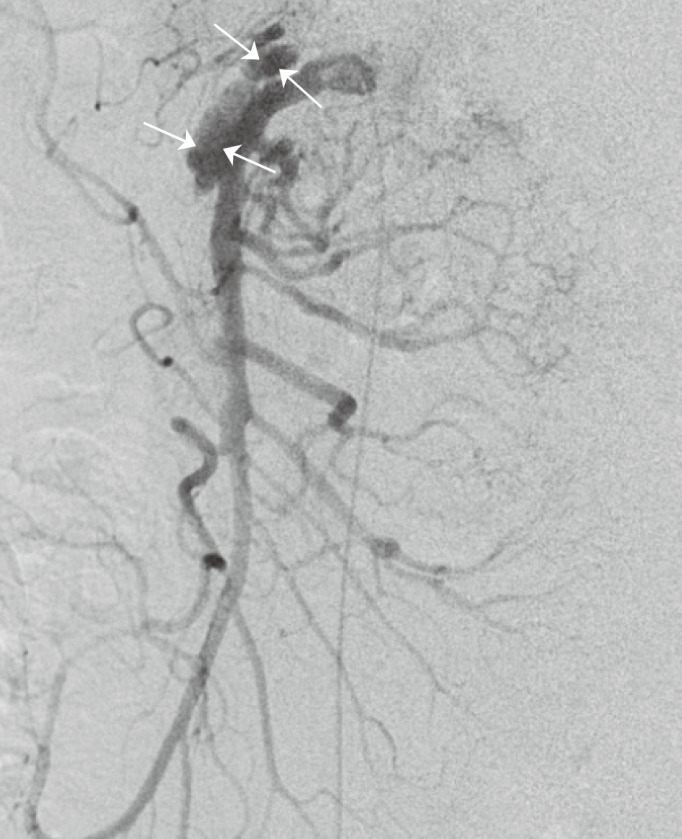
The Classification and Management Strategy of Spontaneous Isolated Superior Mesenteric Artery Dissection
- Affiliations
-
- 1Department of Interventional Radiography, No. 2 People's Hospital of Changzhou, Nanjing Medical University, Chang zhou, China. 747094035@qq.com
- 2Department of Radiology and Interventional Radiology, Lishui Central Hospital, Lishui, China.
- KMID: 2392876
- DOI: http://doi.org/10.4070/kcj.2016.0237
Abstract
- Spontaneous isolated superior mesenteric artery dissection (SISMAD) is an uncommon but potentially catastrophic pathology. Multiple classification schemes have been proposed for this occurrence. Although no consensus has emerged regarding which classification should be used, Li's classification scheme is more precise and complete compared to other classification systems and can be used to guide the treatment of SISMAD. Initial conservative treatment is promising, with favorable early and long-term outcomes for most patients; endovascular treatment is recommended for patients with persistent/recurrent symptoms after conservative treatment; surgical treatment should be performed without delay for patients with arterial rupture, intestinal necrosis, or failed endovascular treatment.
Figure
Reference
-
1. Jia ZZ, Zhao JW, Tian F, et al. Initial and middle-term results of treatment for symptomatic spontaneous isolated dissection of superior mesenteric artery. Eur J Vasc Endovasc Surg. 2013; 45:502–508. PMID: 23481411.2. Kim HK, Jung HK, Cho J, Lee JM, Huh S. Clinical and radiologic course of symptomatic spontaneous isolated dissection of the superior mesenteric artery treated with conservative management. J Vasc Surg. 2014; 59:465–472. PMID: 24080130.3. Luan JY, Li X, Li TR, Zhai GJ, Han JT. Vasodilator and endovascular therapy for isolated superior mesenteric artery dissection. J Vasc Surg. 2013; 57:1612–1620. PMID: 23538008.4. Tomita K, Obara H, Sekimoto Y, et al. Evolution of computed tomographic characteristics of spontaneous isolated superior mesenteric artery dissection during conservative management. Circ J. 2016; 80:1452–1459. PMID: 27118619.5. Bauersfeld SR. Dissecting aneurysm of the aorta; a presentation of 15 cases and a review of the recent literature. Ann Intern Med. 1947; 26:873–889. PMID: 20242656.6. Ogino H. Current treatment strategy for spontaneous isolated dissection of the superior mesenteric artery. Circ J. 2016; 80:1323–1325. PMID: 27194374.7. Sakamoto I, Ogawa Y, Sueyoshi E, Fukui K, Murakami T, Uetani M. Imaging appearances and management of isolated spontaneous dissection of the superior mesenteric artery. Eur J Radiol. 2007; 64:103–110. PMID: 17628380.8. Yun WS, Kim YW, Park KB, et al. Clinical and angiographic follow-up of spontaneous isolated superior mesenteric artery dissection. Eur J Vasc Endovasc Surg. 2009; 37:572–577. PMID: 19208448.9. Zerbib P, Perot C, Lambert M, Seblini M, Pruvot FR, Chambon JP. Management of isolated spontaneous dissection of superior mesenteric artery. Langenbecks Arch Surg. 2010; 395:437–443. PMID: 19588161.10. Luan JY, Li X. Computed tomography imaging features and classification of isolated dissection of the superior mesenteric artery. Eur J Vasc Endovasc Surg. 2013; 46:232–235. PMID: 23746739.11. Li DL, He YY, Alkalei AM, et al. Management strategy for spontaneous isolated dissection of the superior mesenteric artery based on morphologic classification. J Vasc Surg. 2013; 59:165–172. PMID: 23992995.12. Luan JY, Li X. Response to ‘re. computed tomography imaging features and classification of isolated dissection of the superior mesenteric artery’. Eur J Vasc Endovasc Surg. 2014; 47:108–109.13. Nomura Y, Yamaguchi M, Kitagawa A, Okada T, Okita Y, Sugimoto K. Hybrid management of ruptured isolated superior mesenteric artery dissecting aneurysm. J Vasc Surg. 2011; 54:1808–1811. PMID: 21741788.14. Wagenhäuser MU, Sagban TA, Witte M, Duran M, Schelzig H, Oberhuber A. Isolated dissection of the superior mesenteric artery treated using open emergency surgery. World J Emerg Surg. 2014; 9:47. PMID: 25140196.15. Park UJ, Kim HT, Cho WH, Kim YH, Miyata T. Clinical course and angiographic changes of spontaneous isolated superior mesenteric artery dissection after conservative treatment. Surg Today. 2014; 44:2092–2097. PMID: 24496981.16. Li N, Lu QS, Zhou J, Bao JM, Zhao ZQ, Jing ZP. Endovascular stent placement for treatment of spontaneous isolated dissection of the superior mesenteric artery. Ann Vasc Surg. 2014; 28:445–451. PMID: 24070572.17. Sparks SR, Vasquez JC, Bergan JJ, Owens EL. Failure of nonoperative management of isolated superior mesenteric artery dissection. Ann Vasc Surg. 2000; 14:105–109. PMID: 10742422.18. Han Y, Cho YP, Ko GY, et al. Clinical outcomes of anticoagulation therapy in patients with symptomatic spontaneous isolated dissection of the superior mesenteric artery. Medicine (Baltimore). 2016; 95:e3480. PMID: 27100453.19. Garrett HE Jr. Options for treatment of spontaneous mesenteric artery dissection. J Vasc Surg. 2014; 59:1433–1439.e1-2. PMID: 24655752.20. Zhao Y, Yin H, Yao C, et al. Management of acute mesenteric ischemia: a critical review and treatment algorithm. Vasc Endovascular Surg. 2016; 50:183–192. PMID: 27036673.21. Kim YW. Current understandings of spontaneous isolated superior mesenteric artery dissection. Vasc Specialist Int. 2016; 32:37–43. PMID: 27386450.22. Luan JY, Guan X, Li X, et al. Isolated superior mesenteric artery dissection in china. J Vasc Surg. 2016; 63:530–536. PMID: 26597665.23. Leung DA, Schneider E, Kubik-Huch R, Marincek B, Pfammatter T. Acute mesenteric ischemia caused by spontaneous isolated dissection of the superior mesenteric artery: treatment by percutaneous stent placement. Eur Radiol. 2000; 10:1916–1919. PMID: 11305570.24. Min SI, Yoon KC, Min SK, et al. Current strategy for the treatment of symptomatic spontaneous isolated dissection of superior mesenteric artery. J Vasc Surg. 2011; 54:461–466. PMID: 21571493.25. Lee JH, Ahn SG, Yoon J. Endovascular stent grafting via the left radial artery for a spontaneous isolated dissecting rupture of the superior mesenteric artery. Korean Circ J. 2012; 42:140–141. PMID: 22396706.26. Yang HJ, Cho YK, Son TJ, Jung YY, Choi SA, Lee SH. Rapidly aggravated dissecting flap by angiography during percutaneous stent placement for acute isolated superior mesenteric artery dissection. Yonsei Med J. 2011; 52:859–862. PMID: 21786454.27. Chu SY, Hsu MY, Chen CM, et al. Endovascular repair of spontaneous isolated dissection of the superior mesenteric artery. Clin Radiol. 2012; 67:32–37. PMID: 22070946.28. Jia Z, Zhao J, Jiang G. Regarding “management strategy for spontaneous isolated dissection of the superior mesenteric artery based on morphologic classification”. J Vasc Surg. 2014; 59:876–877.29. Sisteron A, Vieville C. Anevrysmes des arteres a destine digestive: Observations personnelles. In : Courbier R, editor. Chirurgie des arterio-pathies digestives. Paris: Expansion Scientifique Francaise;1975. p. 197–202.30. Okamura K, Morizumi S, Kawata M, Suematsu Y. Conservative therapy as a primary treatment for spontaneous isolated dissection of the superior mesenteric artery. Ann Vasc Surg. 2014; 28:1939–1945. PMID: 25048807.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Understandings of Spontaneous Isolated Superior Mesenteric Artery Dissection
- Isolated spontaneous dissection of the superior mesenteric artery
- Spontaneous Isolated Dissection of the Celiac Artery: a Case Report
- Isolated Spontaneous Dissection of the Proximal Superior Mesenteric Artery
- Isolated Spontaneous Dissection of the Superior Mesenteric Artery: Percutaneous Stent Placement in Two Patients