Korean J Pain.
2010 Mar;23(1):78-81.
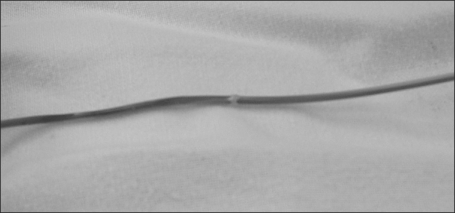
Spontaneous Lead Breakage in Implanted Spinal Cord Stimulation Systems
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University School of Medicine, Seoul, Korea. painfree@snubh.org
Abstract
- Spinal cord stimulation (SCS) has become an established clinical option for treatment of refractory chronic pain. Current hardware and implantation techniques for SCS are already highly developed and continuously improving; however, equipment failures over the course of long-term treatment are still encountered in a relatively high proportion of the cases treated with it. Percutaneous SCS leads seem to be particularly prone to dislocation and insulation failures. We describe our experience of lead breakage in the inserted spinal cord stimulator to a complex regional pain syndrome patient who obtained satisfactory pain relief after the revision of SCS.
Keyword
Figure
Reference
-
1. Kim WY, Moon DE, Choi JH, Park CM, Han SM, Kim SH. The effect of spinal cord stimulation in patients with complex regional pain syndrome. Korean J Pain. 2006; 19:152–158.
Article2. Kumar K, Wilson JR, Taylor RS, Gupta S. Complications of spinal cord stimulation, suggestions to improve outcome, and financial impact. J Neurosurg Spine. 2006; 5:191–203. PMID: 16961079.
Article3. North RB, Wetzel FT. Spinal cord stimulation for chronic pain of spinal origin: a valuable long-term solution. Spine. 2002; 27:2584–2591. PMID: 12435997.
Article4. Oakley JC. Spinal cord stimulation: patient selection, technique, and outcomes. Neurosurg Clin N Am. 2003; 14:365–380. PMID: 14567138.
Article5. Quigley DG, Arnold J, Eldridge PR, Cameron H, McIvor K, Miles JB, et al. Long-term outcome of spinal cord stimulation and hardware complications. Stereotact Funct Neurosurg. 2003; 81:50–56. PMID: 14742964.
Article6. North RB, Kidd DH, Zahurak M, James CS, Long DM. Spinal cord stimulation for chronic, intractable pain: experience over two decades. Neurosurgery. 1993; 32:384–394. PMID: 8455763.7. Taylor RS, Van Buyten JP, Buchser E. Spinal cord stimulation for chronic back and leg pain and failed back surgery syndrome: a systematic review and analysis of prognostic factors. Spine. 2005; 30:152–160. PMID: 15626996.
Article8. ten Vaarwerk IA, Staal MJ. Spinal cord stimulation in chronic pain syndromes. Spinal Cord. 1998; 36:671–682. PMID: 9800271.
Article9. Turner JA, Loeser JD, Deyo RA, Sanders SB. Spinal cord stimulation for patients with failed back surgery syndrome or complex regional pain syndrome: a systematic review of effectiveness and complications. Pain. 2004; 108:137–147. PMID: 15109517.
Article10. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004; 100(3 Suppl):254–267. PMID: 15029914.
Article11. Turner JA, Loeser JD, Bell KG. Spinal cord stimulation for chronic low back pain: a systematic literature synthesis. Neurosurgery. 1995; 37:1088–1095. PMID: 8584149.12. Rainov NG, Heidecke V. Hardware failures in spinal cord stimulation (SCS) for chronic benign pain of spinal origin. Acta Neurochir Suppl. 2007; 97:101–104. PMID: 17691363.
Article13. Henderson JM, Schade CM, Sasaki J, Caraway DL, Oakley JC. Prevention of mechanical failures in implanted spinal cord stimulation systems. Neuromodulation. 2006; 9:183–191.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lead Breakage in Implanted Spinal Cord Stimulation Systems: A case report
- A Case of Lead Migration Caused by Involuntary Movement in Implanted Spinal Cord Stimulation
- Cervical Spinal Cord Stimulation Using an 8 Electrode Lead in a Patient with Complex Regional Pain Syndrome Type I: A case report
- Experience with Spinal Cord Stimulation for Relief of Causalgia on the Right Lower Extremity: A case report
- Spontaneous Herniation of the Thoracic Spinal Cord: A Case Report