Ann Rehabil Med.
2017 Apr;41(2):211-217. 10.5535/arm.2017.41.2.211.
Relationship Between Motor Evoked Potential Response and the Severity of Paralysis in Spinal Cord Injury Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Rehabilitation Medicine, National Rehabilitation Hospital, Seoul, Korea.
- 3Department of Rehabilitation Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. wondol77@gmail.com
- KMID: 2389478
- DOI: http://doi.org/10.5535/arm.2017.41.2.211
Abstract
OBJECTIVE
To investigate the relationship between motor evoked potential (MEP) response and the severity of motor paralysis, evaluated according to the Korean disability evaluation system in patients with spinal cord injury (SCI).
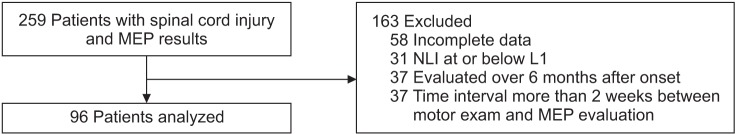
METHODS
We analyzed 192 lower limbs of 96 SCI patients. Lower limbs were classified according to their motor scores, as determined by the International Standards for Neurological Classification of Spinal Cord Injury: motor score <10 (group 1); ≥10 and <15 (group 2); ≥15 and <20 (group 3); and ≥20 (group 4). MEP responses were classified as "˜normal', "˜delayed' or "˜absent', based on their onset latency, which was compared between the different motor score groups.
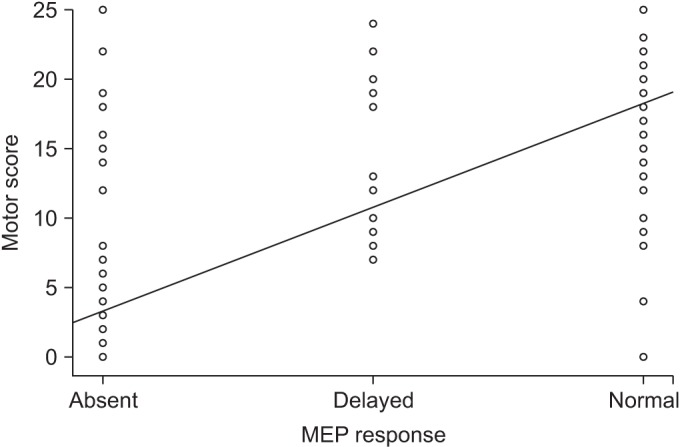
RESULTS
MEP responses and limb motor scores were highly correlated (p<0.001). There was a significant difference of MEP responses between the motor score groups (p<0.001). MEP response was markedly poorer in motor group 1 (limb motor score <10) than in the other three groups (p<0.0001). However, there were no differences between the three groups with motor scores of 10 or above.
CONCLUSION
Clinical utility of MEP as a complimentary tool to manual muscle tests could be limited to discriminating motor score groups with severe paralysis, i.e., single lower limb motor power grades of 0 or 1, and from grade 2, 3, and 4, or above, in the Korean disability evaluation system.
MeSH Terms
Figure
Reference
-
1. Gianutsos J, Eberstein A, Ma D, Holland T, Goodgold J. A noninvasive technique to assess completeness of spinal cord lesions in humans. Exp Neurol. 1987; 98:34–40. PMID: 3653332.
Article2. Berardelli A, Inghilleri M, Manfredi M, Zamponi A, Cecconi V, Dolce G. Cortical and cervical stimulation after hemispheric infarction. J Neurol Neurosurg Psychiatry. 1987; 50:861–865. PMID: 3625209.
Article3. Maertens de Noordhout A, Remacle JM, Pepin JL, Born JD, Delwaide PJ. Magnetic stimulation of the motor cortex in cervical spondylosis. Neurology. 1991; 41:75–80. PMID: 1985298.
Article4. Tavy DL, Wagner GL, Keunen RW, Wattendorff AR, Hekster RE, Franssen H. Transcranial magnetic stimulation in patients with cervical spondylotic myelopathy: clinical and radiological correlations. Muscle Nerve. 1994; 17:235–241. PMID: 8114794.
Article5. Escudero JV, Sancho J, Bautista D, Escudero M, Lopez-Trigo J. Prognostic value of motor evoked potential obtained by transcranial magnetic brain stimulation in motor function recovery in patients with acute ischemic stroke. Stroke. 1998; 29:1854–1859. PMID: 9731608.
Article6. Tavy DL, Franssen H, Keunen RW, Wattendorff AR, Hekster RE, Van Huffelen AC. Motor and somatosensory evoked potentials in asymptomatic spondylotic cord compression. Muscle Nerve. 1999; 22:628–634. PMID: 10331363.
Article7. Nakamae T, Tanaka N, Nakanishi K, Fujimoto Y, Sasaki H, Kamei N, et al. Quantitative assessment of myelopathy patients using motor evoked potentials produced by transcranial magnetic stimulation. Eur Spine J. 2010; 19:685–690. PMID: 20033461.
Article8. Voitenkov VB, Klimkin AV, Skripchenko NV, Pulman NF, Ivanova MV. Diagnostic transcranial magnetic stimulation as a prognostic tool in children with acute transverse myelitis. Spinal Cord. 2016; 54:226–228. PMID: 26238314.
Article9. Curt A, Keck ME, Dietz V. Functional outcome following spinal cord injury: significance of motor-evoked potentials and ASIA scores. Arch Phys Med Rehabil. 1998; 79:81–86. PMID: 9440423.
Article10. Kalita J, Misra UK, Mandal SK. Prognostic predictors of acute transverse myelitis. Acta Neurol Scand. 1998; 98:60–63. PMID: 9696529.
Article11. Raineteau O, Schwab ME. Plasticity of motor systems after incomplete spinal cord injury. Nat Rev Neurosci. 2001; 2:263–273. PMID: 11283749.
Article12. Filli L, Schwab ME. Structural and functional reorganization of propriospinal connections promotes functional recovery after spinal cord injury. Neural Regen Res. 2015; 10:509–513. PMID: 26170799.
Article13. Stenudd M, Sabelstrom H, Frisen J. Role of endogenous neural stem cells in spinal cord injury and repair. JAMA Neurol. 2015; 72:235–237. PMID: 25531583.
Article14. Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011; 34:535–546. PMID: 22330108.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes of motor evoked potentials and spinal cord evoked potentials following spinal cord injury in rats
- Motor Evoked Potentials and Recovery of Motor Function in Spinal Cord Injuried Rats
- Clinical Value of the Somatosensory Evoked Potential in Spinal Cord Injuries
- Spinal Cord Injury
- The Significance of Evoked Potentials according to the Injury Severity of Spinal Cord Contusive Rat Model