J Korean Assoc Oral Maxillofac Surg.
2017 Jun;43(3):152-159. 10.5125/jkaoms.2017.43.3.152.
Skeletal stability following mandibular advancement: is it influenced by the magnitude of advancement or changes of the mandibular plane angle?
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran. tabmed@gmail.com
- 2Student Research Committee, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran.
- 3Department of Oral and Maxillofacial Surgery, School of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran.
- KMID: 2386359
- DOI: http://doi.org/10.5125/jkaoms.2017.43.3.152
Abstract
OBJECTIVES
The aim of this study was to investigate the effects of advancement magnitude and changes in mandibular plane angle on the stability of mandibular advancement.
MATERIALS AND METHODS
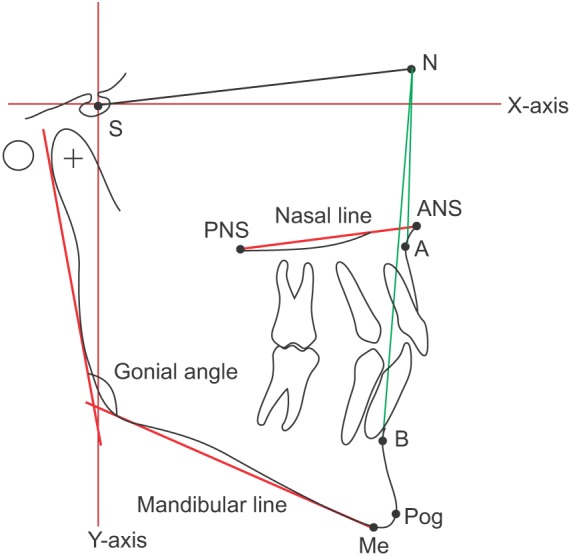
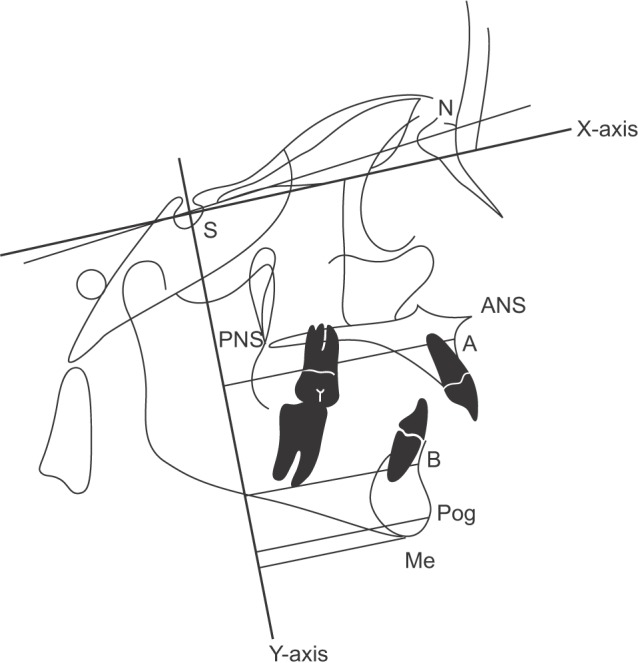
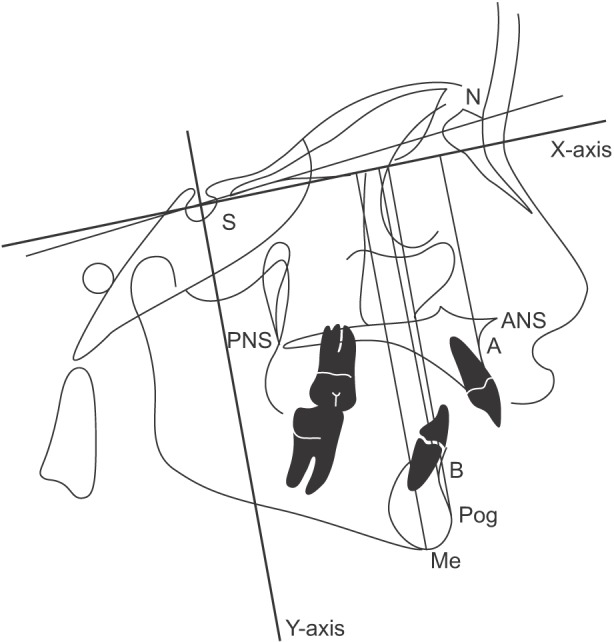
This retrospective cohort study evaluated the postoperative stability of mandibular advancement in class II skeletal subjects who underwent bilateral sagittal split osteotomy. Radiographs taken preoperatively, immediately postoperatively and 1 year postoperatively were traced and analyzed using linear and angular measurements. To determine horizontal and vertical relapse, an X-Y coordinate system was established in which the X-axis was constructed by rotating S-N downward by 7° (approximation of the Frankfort horizontal plane) and the Y-axis was defined as a line perpendicular to the X-axis and passing through the point Sella. For certain reference points including point A, point B, pogonion and menton, the perpendicular distance between each point and both axes was determined and cephalometric variables were recorded as X and Y coordinates.
RESULTS
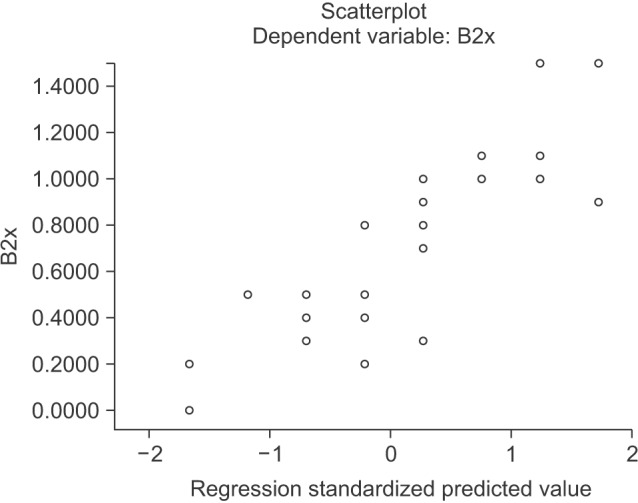
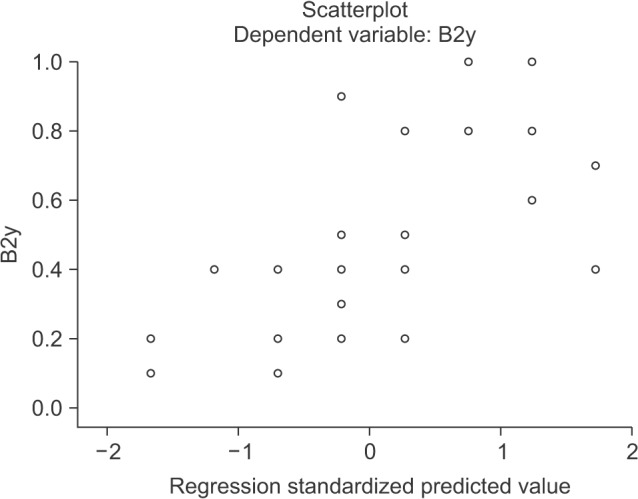
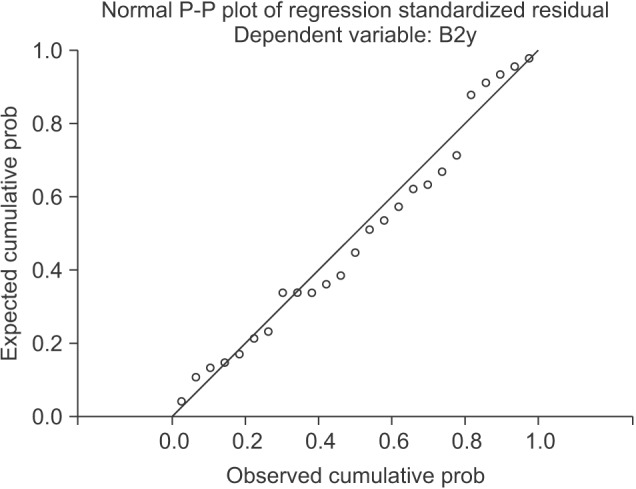
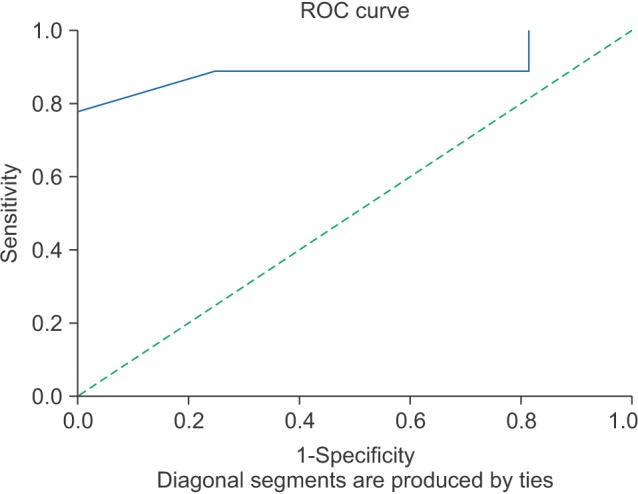
Twenty-five subjects were studied. A significant correlation between the amount of mandibular advancement and relapse in the B point (vertical and horizontal) and the pogonion point was observed (vertical and horizontal, P<0.001). Evaluation of data demonstrated a positive correlation between the mandibular plane angle (SN/ML) change and vertical relapse in the B point (P<0.05). A simple regression model demonstrated that 74% of horizontal relapse and 42.3% of vertical relapse in the B point was related to the amount of mandibular advancement. The receiver operating characteristic test showed that 8.5 mm mandibular advancement is related to a relapse rate of 1 mm or more in the pogonion, vertically or horizontally.
CONCLUSION
The magnitude of mandibular advancement is a stronger surgical predictor for horizontal rather than vertical relapse at the B point. Changes in mandibular plane angle (SN/ML) during surgery affect vertical, but not horizontal relapse at the B point.
MeSH Terms
Figure
Reference
-
1. Oba Y, Yasue A, Kaneko K, Uchida R, Shioyasono A, Moriyama K. Comparison of stability of mandibular segments following the sagittal split ramus osteotomy with poly-l-lactic acid (PLLA) screws and titanium screws fixation. Orthodc Waves. 2008; 67:1–8.
Article2. Moen K, Wisth PJ, Skaale S, Bøe OE, Tornes K. Dental or skeletal relapse after sagittal split osteotomy advancement surgery? Long-term follow-up. J Oral Maxillofac Surg. 2011; 69:e461–e468. PMID: 21741141.
Article3. Pangrazio-Kulbersh V, Berger JL, Kaczynski R, Shunock M. Stability of skeletal Class II correction with 2 surgical techniques: the sagittal split ramus osteotomy and the total mandibular subapical alveolar osteotomy. Am J Orthod Dentofacial Orthop. 2001; 120:134–143. PMID: 11500654.
Article4. Berger JL, Pangrazio-Kulbersh V, Bacchus SN, Kaczynski R. Stability of bilateral sagittal split ramus osteotomy: rigid fixation versus transosseous wiring. Am J Orthod Dentofacial Orthop. 2000; 118:397–403. PMID: 11029735.
Article5. Hoffmannová J, Foltán R, Vlk M, Klíma K, Pavlíková G, Bulik O. Factors affecting the stability of bilateral sagittal split osteotomy of a mandible. Prague Med Rep. 2008; 109:286–297.6. Perrott DH, Lu YF, Pogrel MA, Kaban LB. Stability of sagittal split osteotomies. A comparison of three stabilization techniques. Oral Surg Oral Med Oral Pathol. 1994; 78:696–704. PMID: 7898905.7. Rao SH, Selvaraj L, Lankupalli AS. Skeletal stability after bilateral sagittal split advancement and setback osteotomy of the mandible with miniplate fixation. Craniomaxillofac Trauma Reconstr. 2014; 7:9–16. PMID: 24624252.
Article8. Eggensperger N, Smolka K, Luder J, Iizuka T. Short- and long-term skeletal relapse after mandibular advancement surgery. Int J Oral Maxillofac Surg. 2006; 35:36–42. PMID: 16344217.
Article9. den Besten CA, Mensink G, van Merkesteyn JP. Skeletal stability after mandibular advancement in bilateral sagittal split osteotomies during adolescence. J Craniomaxillofac Surg. 2013; 41:e78–e82. PMID: 23253633.
Article10. Oguz Y, Saglam H, Dolanmaz D, Uckan S. Comparison of stability of 2.0 mm standard and 2.0 mm locking miniplate/screws for the fixation of sagittal split ramus osteotomy on sheep mandibles. Br J Oral Maxillofac Surg. 2011; 49:135–137. PMID: 20226575.11. Eggensperger N, Smolka W, Rahal A, Iizuka T. Skeletal relapse after mandibular advancement and setback in single-jaw surgery. J Oral Maxillofac Surg. 2004; 62:1486–1496. PMID: 15573348.
Article12. Frey DR, Hatch JP, Van Sickels JE, Dolce C, Rugh JD. Alteration of the mandibular plane during sagittal split advancement: short- and long-term stability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:160–169. PMID: 17428696.
Article13. Van Sickels JE, Larsen AJ, Thrash WJ. A retrospective study of relapse in rigidly fixated sagittal split osteotomies: contributing factors. Am J Orthod Dentofacial Orthop. 1988; 93:413–418. PMID: 3163220.
Article14. Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg. 2009; 67:301–313. PMID: 19138603.
Article15. Van Sickels JE. A comparative study of bicortical screws and suspension wires versus bicortical screws in large mandibular advancements. J Oral Maxillofac Surg. 1991; 49:1293–1298. PMID: 1955921.
Article16. Kierl MJ, Nanda RS, Currier GF. A 3-year evaluation of skeletal stability of mandibular advancement with rigid fixation. J Oral Maxillofac Surg. 1990; 48:587–592. PMID: 2341939.
Article17. Scheerlinck JP, Stoelinga PJ, Blijdorp PA, Brouns JJ, Nijs ML. Sagittal split advancement osteotomies stabilized with miniplates. A 2-5-year follow-up. Int J Oral Maxillofac Surg. 1994; 23:127–131. PMID: 7930763.
Article18. Kallela I, Laine P, Suuronen R, Iizuka T, Pirinen S, Lindqvist C. Skeletal stability following mandibular advancement and rigid fixation with polylactide biodegradable screws. Int J Oral Maxillofac Surg. 1998; 27:3–8. PMID: 9506290.
Article19. Arpornmaeklong P, Shand JM, Heggie AA. Skeletal stability following maxillary impaction and mandibular advancement. Int J Oral Maxillofac Surg. 2004; 33:656–663. PMID: 15337178.
Article20. Bouwman JP, Tuinzing DB, Kostense PJ, van Teeseling RA, Mokhtari H. The value of long-term follow-up of mandibular advancement surgery in patients with a low to normal mandibular plane angle. Mund Kiefer Gesichtschir. 1997; 1:311–315. PMID: 9433095.
Article21. Emshoff R, Scheiderbauer A, Gerhard S, Norer B. Stability after rigid fixation of simultaneous maxillary impaction and mandibular advancement osteotomies. Int J Oral Maxillofac Surg. 2003; 32:137–142. PMID: 12729772.
Article22. Mobarak KA, Espeland L, Krogstad O, Lyberg T. Mandibular advancement surgery in high-angle and low-angle class II patients: different long-term skeletal responses. Am J Orthod Dentofacial Orthop. 2001; 119:368–381. PMID: 11298310.
Article23. Ow A, Cheung LK. Skeletal stability and complications of bilateral sagittal split osteotomies and mandibular distraction osteogenesis: an evidence-based review. J Oral Maxillofac Surg. 2009; 67:2344–2353. PMID: 19837301.
Article24. Yoshida K, Rivera GA, Matsuo N, Takaishi M, Inamoto H, Kurita K. Long-term prognosis of BSSO mandibular relapse and its relation to different facial types. Angle Orthod. 2000; 70:220–226. PMID: 10926431.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors affecting postsurgical stability in skeletal Class III malocclusion patients
- A comparative study of initial lateral cephalometric characteristics: mandibular setback surgery only versus mandibular setback surgery with advancement genioplasty
- Microimplant mandibular advancement (MiMA) therapy for the treatment of snoring and obstructive sleep apnea (OSA)
- Does maxillomandibular fixation affect skeletal stability following mandibular advancement? A single-blind clinical trial
- Postoperative stability and occlusal plane alternation by orthgnathic surgery of skeletal Class III malocclusion with anterior open bite