Korean J Pain.
2017 Jul;30(3):183-191. 10.3344/kjp.2017.30.3.183.
Low doses of amitriptyline, pregabalin, and gabapentin are preferred for management of neuropathic pain in India: is there a need for revisiting dosing recommendations?
- Affiliations
-
- 1Medical Affairs Department, Wockhardt Limited, Wockhardt Towers, Bandra Kurla Complex, Mumbai, India. skamble@wockhardt.com
- KMID: 2385350
- DOI: http://doi.org/10.3344/kjp.2017.30.3.183
Abstract
- BACKGROUND
Current therapy for the treatment of neuropathic pain is often unsatisfactory. Considerable variation in treatment pattern still exists in spite of availability of sufficient literature from various guidelines. Recent Indian market data suggested that the utilization (sale) of drugs such as amitriptyline, pregabalin, and gabapentin was more for low-dose unit packs than that of the high-dose unit packs, raising the belief that these drugs are prescribed at a lower dose than is actually recommended in the guidelines. To test this hypothesis, a survey was conducted across speciality throughout the country to observe the prescription pattern of these drugs amongst the health care providers in India.
METHODS
Three hundred fifty survey forms were distributed of which 281 forms were included for analysis.
RESULTS
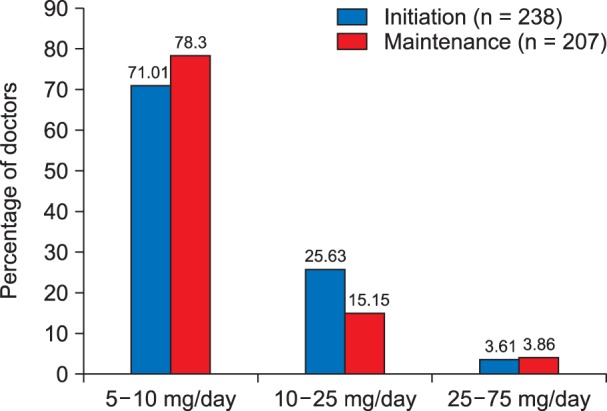
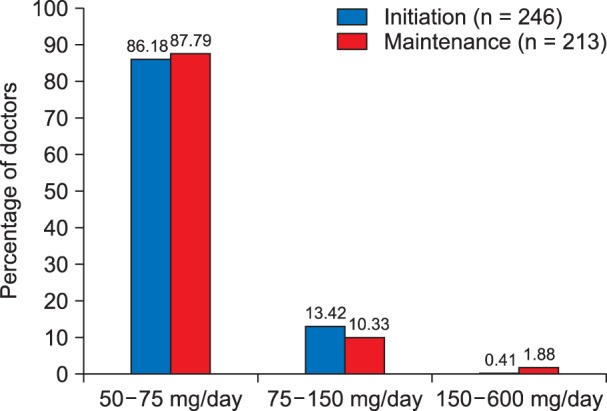
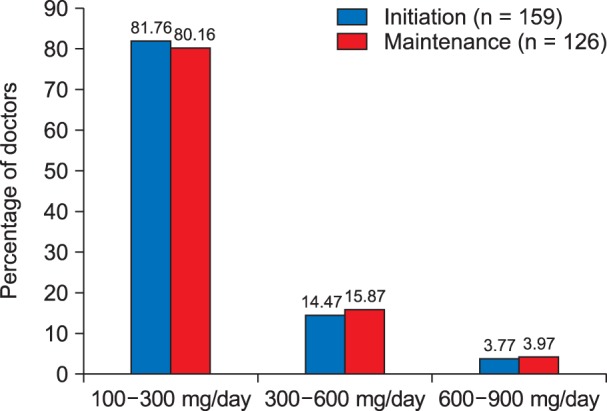
It was observed that the commonly used initiation and maintenance dose for amitriptyline, pregabalin, and gabapentin was 5-10 mg/day, 50-75 mg/day, and 100-300 mg/day, respectively. The reason to select the lower dosages was to have a balancing effect to achieve good efficacy with minimum side effects. Care-givers reported no side effects/not many side effects as a reason in 22.2%, 16.88%, and 23.86% patients with amitriptyline, pregabalin, and gabapentin, respectively. Sedation and giddiness were commonly reported with all three drugs.
CONCLUSIONS
Commonly prescribed drugs for management of neuropathic pain, such as amitriptyline, pregabalin, and gabapentin are preferred at lower doses in Indian clinical settings. Acceptable efficacy and low tolerance to the standard dosage is believed to be the reason behind the prescribed dose.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Pregabalin and gabapentin in neuropathic pain management after spinal cord injury: a systematic review and meta-analysis
Majid Davari, Bahman Amani, Behnam Amani, Ahmad Khanijahani, Arash Akbarzadeh, Rouhollah Shabestan
Korean J Pain. 2020;33(1):3-12. doi: 10.3344/kjp.2020.33.1.3.
Reference
-
1. Nascimento OJ, Pessoa BL, Orsini M, Ribeiro P, Davidovich E, Pupe C, et al. Neuropathic pain treatment: still a challenge. Neurol Int. 2016; 8:6322. PMID: 27441065.
Article2. Campbell JN, Meyer RA. Mechanisms of neuropathic pain. Neuron. 2006; 52:77–92. PMID: 17015228.
Article3. Dworkin RH, O'Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010; 85:S3–S14.
Article4. Moulin D, Boulanger A, Clark AJ, Clarke H, Dao T, Finley GA, et al. Pharmacological management of chronic neuropathic pain: revised consensus statement from the Canadian pain society. Pain Res Manag. 2014; 19:328–335. PMID: 25479151.
Article5. Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010; 17:1113–1e88. PMID: 20402746.
Article6. NICE. Neuropathic pain: the pharmacological management of neuropathic pain in adults in non-specialist settings. Centre for clinical practice at NICE (UK). London: National Institute for Health and Clinical Excellence (UK);2010. p. 1–138.7. Liu Y, Qian C, Yang M. Treatment patterns associated with ACR-recommended medications in the management of Fibromyalgia in the United States. J Manag Care Spec Pharm. 2016; 22:263–271. PMID: 27003556.
Article8. Park HJ, Moon DE. Pharmacologic management of chronic pain. Korean J Pain. 2010; 23:99–108. PMID: 20556211.
Article9. Quintiles IMS Sales Data (Total Sales Audit and Secondary Sales Audit): Indian Pharmaceutical Market; Amitripyline, Gabapentin & Pregabalin; Moving Annual Total (MAT). 2016. 8.10. Bockbrader HN, Wesche D, Miller R, Chapel S, Janiczek N, Burger P. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010; 49:661–669. PMID: 20818832.
Article11. Nantz E, Liu-Seifert H, Skljarevski V. Predictors of premature discontinuation of treatment in multiple disease states. Patient Prefer Adherence. 2009; 3:31–43. PMID: 19936143.
Article12. Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005; 116:109–118. PMID: 15927394.
Article13. Richter RW, Portenoy R, Sharma U, Lamoreaux L, Bockbrader H, Knapp LE. Relief of painful diabetic neuropathy with pregabalin: a randomized, placebo-controlled trial. J Pain. 2005; 6:253–260. PMID: 15820913.
Article14. Backonja M, Glanzman RL. Gabapentin dosing for neuropathic pain: evidence from randomized, placebo-controlled clinical trials. Clin Ther. 2003; 25:81–104. PMID: 12637113.
Article15. Dogra S, Beydoun S, Mazzola J, Hopwood M, Wan Y. Oxcarbazepine in painful diabetic neuropathy: a randomized, placebo-controlled study. Eur J Pain. 2005; 9:543–554. PMID: 16139183.
Article16. Vinik AI, Tuchman M, Safirstein B, Corder C, Kirby L, Wilks K, et al. Lamotrigine for treatment of pain associated with diabetic neuropathy: results of two randomized, double-blind, placebo-controlled studies. Pain. 2007; 128:169–179. PMID: 17161535.
Article17. Patkar AA, Masand PS, Krulewicz S, Mannelli P, Peindl K, Beebe KL, et al. A randomized, controlled, trial of controlled release paroxetine in fibromyalgia. Am J Med. 2007; 120:448–454. PMID: 17466657.
Article18. Arnold LM, Goldenberg DL, Stanford SB, Lalonde JK, Sandhu HS, Keck PE Jr, et al. Gabapentin in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled, multi-center trial. Arthritis Rheum. 2007; 56:1336–1344. PMID: 17393438.
Article19. Crofford LJ, Rowbotham MC, Mease PJ, Russell IJ, Dworkin RH, Corbin AE, et al. Pregabalin for the treatment of fibromyalgia syndrome: results of a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2005; 52:1264–1273. PMID: 15818684.
Article20. Arnold LM, Crofford LJ, Martin SA, Young JP, Sharma U. The effect of anxiety and depression on improvements in pain in a randomized, controlled trial of pregabalin for treatment of fibromyalgia. Pain Med. 2007; 8:633–638. PMID: 18028041.
Article21. Agius AM, Jones NS, Muscat R. A randomized controlled trial comparing the efficacy of low-dose amitriptyline, amitriptyline with pindolol and surrogate placebo in the treatment of chronic tension-type facial pain. Rhinology. 2013; 51:143–153. PMID: 23671895.
Article22. Kautio AL, Haanpää M, Saarto T, Kalso E. Amitriptyline in the treatment of chemotherapy-induced neuropathic symptoms. J Pain Symptom Manage. 2008; 35:31–39. PMID: 17980550.
Article23. Bowsher D. The management of postherpetic neuralgia. Postgrad Med J. 1997; 73:623–629. PMID: 9497970.
Article24. Kulshreshtha P, Gupta R, Yadav RK, Bijlani RL, Deepak KK. Effect of low-dose amitriptyline on autonomic functions and peripheral blood flow in fibromyalgia: a pilot study. Pain Med. 2012; 13:131–136. PMID: 22142408.
Article25. Freysoldt A, Fleckenstein J, Lang PM, Irnich D, Grafe P, Carr RW. Low concentrations of amitriptyline inhibit nicotinic receptors in unmyelinated axons of human peripheral nerve. Br J Pharmacol. 2009; 158:797–805. PMID: 19694730.
Article26. George RB, McKeen DM, Andreou P, Habib AS. A randomized placebo-controlled trial of two doses of pregabalin for postoperative analgesia in patients undergoing abdominal hysterectomy. Can J Anaesth. 2014; 61:551–557. PMID: 24668315.
Article27. Khurana G, Jindal P, Sharma JP, Bansal KK. Postoperative pain and long-term functional outcome after administration of gabapentin and pregabalin in patients undergoing spinal surgery. Spine (Phila Pa 1976). 2014; 39:E363–E368. PMID: 24384657.
Article28. Nishihara M, Arai YC, Yamamoto Y, Nishida K, Arakawa M, Ushida T, et al. Combinations of low-dose antidepressants and low-dose pregabalin as useful adjuvants to opioids for intractable, painful bone metastases. Pain Physician. 2013; 16:E547–E552. PMID: 24077205.29. Zin CS, Nissen LM, O’Callaghan JP, Duffull SB, Smith MT, Moore BJ. A randomized, controlled trial of oxycodone versus placebo in patients with postherpetic neuralgia and painful diabetic neuropathy treated with pregabalin. J Pain. 2010; 11:462–471. PMID: 19962354.
Article30. Hounnou P, Nicoucar K. Delayed onset of rotatory self-motion perception, dysdiadochokinesia and disturbed eye pursuit caused by low-dose pregabalin. BMJ Case Rep. 2014; 4. 11. [serial on the Internet]. Available at http://casereports.bmj.com/content/2014/bcr-2013-201282.long.
Article31. Peng PW, Li C, Farcas E, Haley A, Wong W, Bender J, et al. Use of low-dose pregabalin in patients undergoing laparoscopic cholecystectomy. Br J Anaesth. 2010; 105:155–161. PMID: 20581215.
Article32. Randinitis EJ, Posvar EL, Alvey CW, Sedman AJ, Cook JA, Bockbrader HN. Pharmacokinetics of pregabalin in subjects with various degrees of renal function. J Clin Pharmacol. 2003; 43:277–283. PMID: 12638396.
Article33. Semel D, Murphy TK, Zlateva G, Cheung R, Emir B. Evaluation of the safety and efficacy of pregabalin in older patients with neuropathic pain: results from a pooled analysis of 11 clinical studies. BMC Fam Pract. 2010; 11:85. PMID: 21054853.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pregabalin versus Gabapentin Efficacy in the Management of Neuropathic Pain Associated with Failed Back Surgery Syndrome
- Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy
- Mirogabalin: could it be the next generation gabapentin or pregabalin?
- Comparison of pretreatment gabapentin and pregabalin to control postoperative endodontic pain – a double-blind, randomized clinical trial
- Experience with Gabapentin for Neuropathic Pain