Korean J Pain.
2017 Jul;30(3):165-175. 10.3344/kjp.2017.30.3.165.
Bone scintigraphy in patients with pain
- Affiliations
-
- 1Department of Nuclear Medicine, Pusan National University Hospital, Busan, Korea. growthkim@daum.net
- 2Department of Nuclear Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 3BioMedical Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2385348
- DOI: http://doi.org/10.3344/kjp.2017.30.3.165
Abstract
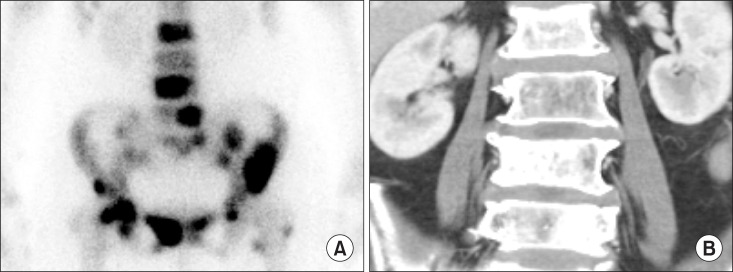
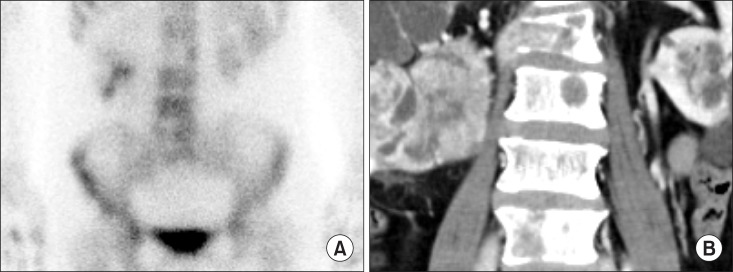
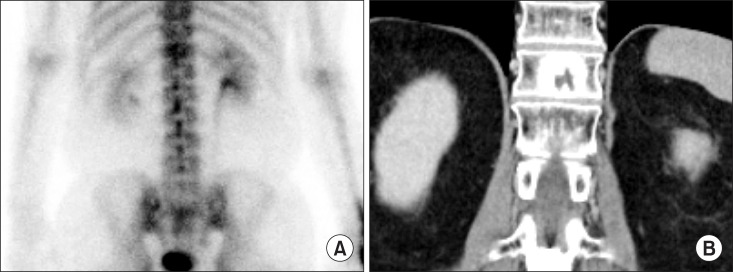
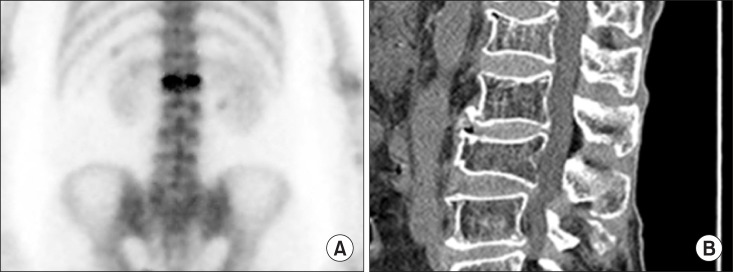
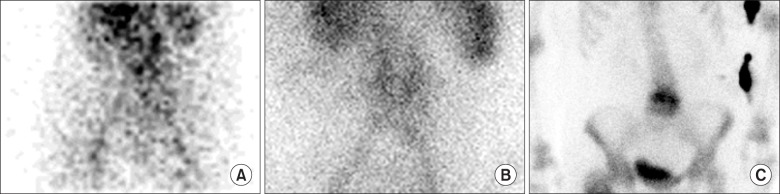
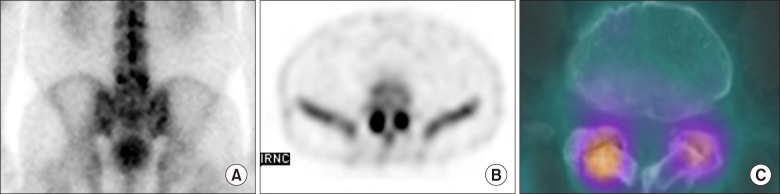
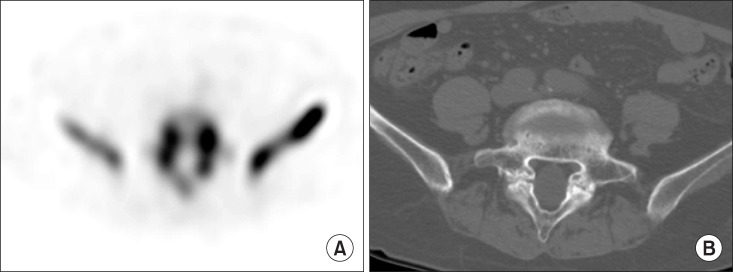
- Nuclear medicine imaging is widely used in pain medicine. Low back pain is commonly encountered by physicians, with its prevalence from 49% to 70%. Computed tomography (CT) or magnetic resonance imaging (MRI) are usually used to evaluate the cause of low back pain, however, these findings from these scans could also be observed in asymptomatic patients. Bone scintigraphy has an additional value in patients with low back pain. Complex regional pain syndrome (CRPS) is defined as a painful disorder of the extremities, which is characterized by sensory, autonomic, vasomotor, and trophic disturbances. To assist the diagnosis of CRPS, three-phase bone scintigraphy is thought to be superior compared to other modalities, and could be used to rule out CRPS due to its high specificity. Studies regarding the effect of bone scintigraphy in patients with extremity pain have not been widely conducted. Ultrasound, CT and MRI are widely used imaging modalities for evaluating extremity pain. However, SPECT/CT has an additional role in assessing pain in the extremities.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Successful removal of permanent spinal cord stimulators in patients with complex regional pain syndrome after complete relief of pain
Su Jung Lee, Yeong Min Yoo, Jun A You, Sang Wook Shin, Tae Kyun Kim, Salahadin Abdi, Kyung Hoon Kim
Korean J Pain. 2019;32(1):47-50. doi: 10.3344/kjp.2019.32.1.47.
Reference
-
1. Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006; 332:1430–1434. PMID: 16777886.
Article2. De Maeseneer M, Lenchik L, Everaert H, Marcelis S, Bossuyt A, Osteaux M, et al. Evaluation of lower back pain with bone scintigraphy and SPECT. Radiographics. 1999; 19:901–912. PMID: 10464798.
Article3. Valdez DC, Johnson RG. Role of technetium-99m planar bone scanning in the evaluation of low back pain. Skeletal Radiol. 1994; 23:91–97. PMID: 8191307.
Article4. Matesan M, Behnia F, Bermo M, Vesselle H. SPECT/CT bone scintigraphy to evaluate low back pain in young athletes: common and uncommon etiologies. J Orthop Surg Res. 2016; 11:76. PMID: 27387155.
Article5. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986; 3:S1–S226. PMID: 3461421.6. Fischer SG, Perez RS. Complex regional pain syndrome-diagnosis, treatment and future perspectives. Eur Neurol Rev. 2011; 6:270–275.
Article7. Goh EL, Chidambaram S, Ma D. Complex regional pain syndrome: a recent update. Burns Trauma. 2017; 5:2. PMID: 28127572.
Article8. Birklein F, O'Neill D, Schlereth T. Complex regional pain syndrome: an optimistic perspective. Neurology. 2015; 84:89–96. PMID: 25471395.
Article9. Stanton-Hicks M, Jänig W, Hassenbusch S, Haddox JD, Boas R, Wilson P. Reflex sympathetic dystrophy: changing concepts and taxonomy. Pain. 1995; 63:127–133. PMID: 8577483.
Article10. Galer BS, Bruehl S, Harden RN. IASP diagnostic criteria for complex regional pain syndrome: a preliminary empirical validation study. International Association for the Study of Pain. Clin J Pain. 1998; 14:48–54. PMID: 9535313.
Article11. Bruehl S, Harden RN, Galer BS, Saltz S, Bertram M, Backonja M, et al. External validation of IASP diagnostic criteria for Complex Regional Pain Syndrome and proposed research diagnostic criteria. International Association for the Study of Pain. Pain. 1999; 81:147–154. PMID: 10353502.
Article12. Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007; 8:326–331. PMID: 17610454.
Article13. Cappello ZJ, Kasdan ML, Louis DS. Meta-analysis of imaging techniques for the diagnosis of complex regional pain syndrome type I. J Hand Surg Am. 2012; 37:288–296. PMID: 22177715.
Article14. Wasner G, Schattschneider J, Binder A, Baron R. Complex regional pain syndrome--diagnostic, mechanisms, CNS involvement and therapy. Spinal Cord. 2003; 41:61–75. PMID: 12595868.
Article15. Humphreys SC, Eck JC, Hodges SD. Neuroimaging in low back pain. Am Fam Physician. 2002; 65:2299–2306. PMID: 12074530.16. Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging. 6th ed. Philiadelphia (PA): Elsevier/Saunders;2012. p. 280.17. O'Sullivan GJ, Carty FL, Cronin CG. Imaging of bone metastasis: an update. World J Radiol. 2015; 7:202–211. PMID: 26339464.18. Ciftdemir M, Kaya M, Selcuk E, Yalniz E. Tumors of the spine. World J Orthop. 2016; 7:109–116. PMID: 26925382.
Article19. Kim JH, Kim JI, Jang BH, Seo JG, Kim JH. The comparison of bone scan and MRI in osteoporotic compression fractures. Asian Spine J. 2010; 4:89–95. PMID: 21165311.
Article20. Maynard AS, Jensen ME, Schweickert PA, Marx WF, Short JG, Kallmes DF. Value of bone scan imaging in predicting pain relief from percutaneous vertebroplasty in osteoporotic vertebral fractures. AJNR Am J Neuroradiol. 2000; 21:1807–1812. PMID: 11110531.21. Vali R, Bajno L, Kousha M, Martin C. The potential role of radionuclide imaging in osteoporotic vertebral fracture and sacral fracture. Spine Res. 2016; 2:11.
Article22. Jun DS, An BK, Yu CH, Hwang KH, Paik JW. Practical use of bone scan in patients with an osteoporotic vertebral compression fracture. J Korean Med Sci. 2015; 30:194–198. PMID: 25653492.
Article23. Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg. 2009; 23:80–89. PMID: 20567730.
Article24. Doutchi M, Seng P, Menard A, Meddeb L, Adetchessi T, Fuentes S, et al. Changing trends in the epidemiology of vertebral osteomyelitis in Marseille, France. New Microbes New Infect. 2015; 7:1–7. PMID: 26110060.
Article25. Jeong SJ, Choi SW, Youm JY, Kim HW, Ha HG, Yi JS. Microbiology and epidemiology of infectious spinal disease. J Korean Neurosurg Soc. 2014; 56:21–27. PMID: 25289121.
Article26. Rotaru N, Pripa V, Punga J, Condrea E, Seu V, Frumusachi O, et al. Nuclear medicine imaging for evaluation of low back pain [Internet]. Dover (DE): SM Group;2016. cited 2017 Jun 25. Available at: http://www.smgebooks.com/neuroimaging/chapters/NI-1 6-07.pdf.27. Love C, Patel M, Lonner BS, Tomas MB, Palestro CJ. Diagnosing spinal osteomyelitis: a comparison of bone and Ga-67 scintigraphy and magnetic resonance imaging. Clin Nucl Med. 2000; 25:963–977. PMID: 11129162.28. Shur N, Corrigan A, Agrawal K, Desai A, Gnanasegaran G. Radiological and radionuclide imaging of degenerative disease of the facet joints. Indian J Nucl Med. 2015; 30:191–198. PMID: 26170560.
Article29. Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD. Spondylolysis: a review and reappraisal. Hippokratia. 2010; 14:17–21. PMID: 20411054.30. Yamaguchi KT Jr, Skaggs DL, Acevedo DC, Myung KS, Choi P, Andras L. Spondylolysis is frequently missed by MRI in adolescents with back pain. J Child Orthop. 2012; 6:237–240. PMID: 23814624.
Article31. Standaert CJ, Herring SA. Spondylolysis: a critical review. Br J Sports Med. 2000; 34:415–422. PMID: 11131228.
Article32. Masci L, Pike J, Malara F, Phillips B, Bennell K, Brukner P. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006; 40:940–946. PMID: 16980534.
Article33. Frühling J, Verbist A, Balikdjian D. Which diphosphonate for routine bone scintigraphy (MDP, HDP or DPD)? Nucl Med Commun. 1986; 7:415–425. PMID: 3748485.
Article34. Okamoto Y. Accumulation of technetium-99m methylene diphosphonate. Conditions affecting adsorption to hydroxyapatite. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:115–119. PMID: 7552850.35. Brenner AI, Koshy J, Morey J, Lin C, DiPoce J. The bone scan. Semin Nucl Med. 2012; 42:11–26. PMID: 22117809.
Article36. Ziessman HA, O'Malley JP, Thrall JH, Fahey H. Nuclear medicine: the requisites. 4th ed. Philadelphia (PA): Elsevier Sunders;2014. p. 100.37. Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics. 2003; 23:341–358. PMID: 12640151.
Article38. Wüppenhorst N, Maier C, Frettlöh J, Pennekamp W, Nicolas V. Sensitivity and specificity of 3-phase bone scintigraphy in the diagnosis of complex regional pain syndrome of the upper extremity. Clin J Pain. 2010; 26:182–189. PMID: 20173431.
Article39. Kwon HW, Paeng JC, Nahm FS, Kim SG, Zehra T, Oh SW, et al. Diagnostic performance of three-phase bone scan for complex regional pain syndrome type 1 with optimally modified image criteria. Nucl Med Mol Imaging. 2011; 45:261–267. PMID: 24900016.
Article40. Ringer R, Wertli M, Bachmann LM, Buck FM, Brunner F. Concordance of qualitative bone scintigraphy results with presence of clinical complex regional pain syndrome 1: meta-analysis of test accuracy studies. Eur J Pain. 2012; 16:1347–1356. PMID: 22473897.
Article41. Wertli MM, Brunner F, Steurer J, Held U. Usefulness of bone scintigraphy for the diagnosis of Complex Regional Pain Syndrome 1: a systematic review and Bayesian meta-analysis. PLoS One. 2017; 12:e0173688. PMID: 28301606.
Article42. Schürmann M, Zaspel J, Löhr P, Wizgall I, Tutic M, Manthey N, et al. Imaging in early posttraumatic complex regional pain syndrome: a comparison of diagnostic methods. Clin J Pain. 2007; 23:449–457. PMID: 17515744.43. Elgazzar AH. Orthopedic nuclear medicine. New York (NY): Springer;2004. p. 88–91.44. Turpin S, Taillefer R, Lambert R, Leveille J. “Cold” reflex sympathetic dystrophy in an adult. Clin Nucl Med. 1996; 21:94–97. PMID: 8697698.
Article45. Low AK, Ward K, Wines AP. Pediatric complex regional pain syndrome. J Pediatr Orthop. 2007; 27:567–572. PMID: 17585269.
Article46. Park JM, Kim SJ, Chung SH, Lee YT. Study for reliability of interpretation of the three phase bone scintigraphy in patients with post-traumatic complex regional pain syndrome. Nucl Med Mol Imaging. 2008; 42:44–51.47. Saha S, Burke C, Desai A, Vijayanathan S, Gnanasegaran G. SPECT-CT: applications in musculoskeletal radiology. Br J Radiol. 2013; 86:20120519. PMID: 24096590.
Article48. Hirschmann MT, Schmid R, Dhawan R, Skarvan J, Rasch H, Friederich NF, et al. Combined single photon emission computerized tomography and conventional computerized tomography: clinical value for the shoulder surgeons? Int J Shoulder Surg. 2011; 5:72–76. PMID: 22058640.
Article49. Walton J, Mahajan S, Paxinos A, Marshall J, Bryant C, Shnier R, et al. Diagnostic values of tests for acromioclavicular joint pain. J Bone Joint Surg Am. 2004; 86-A:807–812. PMID: 15069148.
Article50. Huellner MW, Bürkert A, Schleich FS, Schürch M, Hug U, von Wartburg U, et al. SPECT/CT versus MRI in patients with nonspecific pain of the hand and wrist - a pilot study. Eur J Nucl Med Mol Imaging. 2012; 39:750–759. PMID: 22237845.
Article51. Dreinhöfer KE, Dieppe P, Stürmer T, Gröber-Grätz D, Flören M, Günther KP, et al. Indications for total hip replacement: comparison of assessments of orthopaedic surgeons and referring physicians. Ann Rheum Dis. 2006; 65:1346–1350. PMID: 16439438.
Article52. Palestro CJ. Nuclear medicine and the failed joint replacement: past, present, and future. World J Radiol. 2014; 6:446–458. PMID: 25071885.
Article53. Arıcan P, Okudan Tekin B, Şefizade R, Naldöken S, Baştuğ A, Özkurt B. The role of bone SPECT/CT in the evaluation of painful joint prostheses. Nucl Med Commun. 2015; 36:931–940. PMID: 26049374.
Article54. Temmerman OP, Raijmakers PG, Berkhof J, Hoekstra OS, Teule GJ, Heyligers IC. Accuracy of diagnostic imaging techniques in the diagnosis of aseptic loosening of the femoral component of a hip prosthesis: a meta-analysis. J Bone Joint Surg Br. 2005; 87:781–785. PMID: 15911658.55. Ro DH, Lee HY, Chang CB, Kang SB. Value of SPECT-CT imaging for middle-aged patients with chronic anterior knee pain. BMC Musculoskelet Disord. 2015; 16:169. PMID: 26210673.
Article56. Al-Nabhani K, Michopoulou S, Allie R, Alkalbani J, Saad Z, Sajjan R, et al. Painful knee prosthesis: can we help with bone SPECT/CT? Nucl Med Commun. 2014; 35:182–188. PMID: 24152807.57. Singh VK, Javed S, Parthipun A, Sott AH. The diagnostic value of single photon-emission computed tomography bone scans combined with CT (SPECT-CT) in diseases of the foot and ankle. Foot Ankle Surg. 2013; 19:80–83. PMID: 23548447.
Article58. Ha S, Hong SH, Paeng JC, Lee DY, Cheon GJ, Arya A, et al. Comparison of SPECT/CT and MRI in diagnosing symptomatic lesions in ankle and foot pain patients: diagnostic performance and relation to lesion type. PLoS One. 2015; 10:e0117583. PMID: 25668182.
Article59. Claassen L, Uden T, Ettinger M, Daniilidis K, Stukenborg-Colsman C, Plaass C. Influence on therapeutic decision making of SPECT-CT for different regions of the foot and ankle. Biomed Res Int. 2014; 2014:927576. PMID: 24959593.
Article60. Rosado-de-Castro PH, Lopes de Souza SA, Alexandre D, Barbosa da, Gutfilen B. Rheumatoid arthritis: Nuclear Medicine state-of-the-art imaging. World J Orthop. 2014; 5:312–318. PMID: 25035834.
Article61. Sahin M, Bernay I, Basoglu T, Canturk F. Comparison of Tc-99m MDP, Tc-99m HSA and Tc-99m HIG uptake in rheumatoid arthritis and its variants. Ann Nucl Med. 1999; 13:389–395. PMID: 10656272.
Article62. Berná L, Torres G, Diez C, Estorch M, Martínez-Duncker D, Carrió I. Technetium-99m human polyclonal immunoglobulin G studies and conventional bone scans to detect active joint inflammation in chronic rheumatoid arthritis. Eur J Nucl Med. 1992; 19:173–176. PMID: 1572380.
Article63. Ozgul A, Yasar E, Arslan N, Balaban B, Taskaynatan MA, Tezel K, et al. The comparison of ultrasonographic and scintigraphic findings of early arthritis in revealing rheumatoid arthritis according to criteria of American College of Rheumatology. Rheumatol Int. 2009; 29:765–768. PMID: 19037610.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- (99m)Tc-HDP Bone Scintigraphy Finding of Metastatic Renal Cell Carcinoma Bone Lesion Changed from Hot to Cold Lesion: Comparing with (18)F-FDG PET/CT
- Usefulness of Uptake Ratio of Three Phase Bone Scintigraphy in Complex Regional Pain Syndrome after a Stroke
- Induction of Radiation Adaptive Response in Lymphocytes of patients Undergoing Bone Scintigraphy
- Acute Rhabdomyolysis : Importance of MRI and Bone Scintigraphy
- The Effectiveness of Bone Scintigraphy of Femur neck fracture