J Clin Neurol.
2016 Oct;12(4):446-451. 10.3988/jcn.2016.12.4.446.
Detection of Listeria monocytogenes in CSF from Three Patients with Meningoencephalitis by Next-Generation Sequencing
- Affiliations
-
- 1Department of Neurology, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China. guanhz@263.net
- 2Binhai Genomics Institute, Tianjin Translational Genomics Center, BGI-Tianjin, BGI-Shenzhen, Tianjin, China. wuhonglong@genomics.cn
- 3Neuroscience Center, Chinese Academy of Medical Sciences, Beijing, China.
- 4Wuhan National Laboratory for Optoelectronics, Huazhong University of Science and Technology, Wuhan, Hubei, China.
- KMID: 2385109
- DOI: http://doi.org/10.3988/jcn.2016.12.4.446
Abstract
- BACKGROUND AND PURPOSE
Encephalitis caused by Listeria monocytogenes (L. monocytogenes) is rare but sometimes fatal. Early diagnosis is difficult using routine cerebrospinal fluid (CSF) tests, while next-generation sequencing (NGS) is increasingly being used for the detection and characterization of pathogens.
METHODS
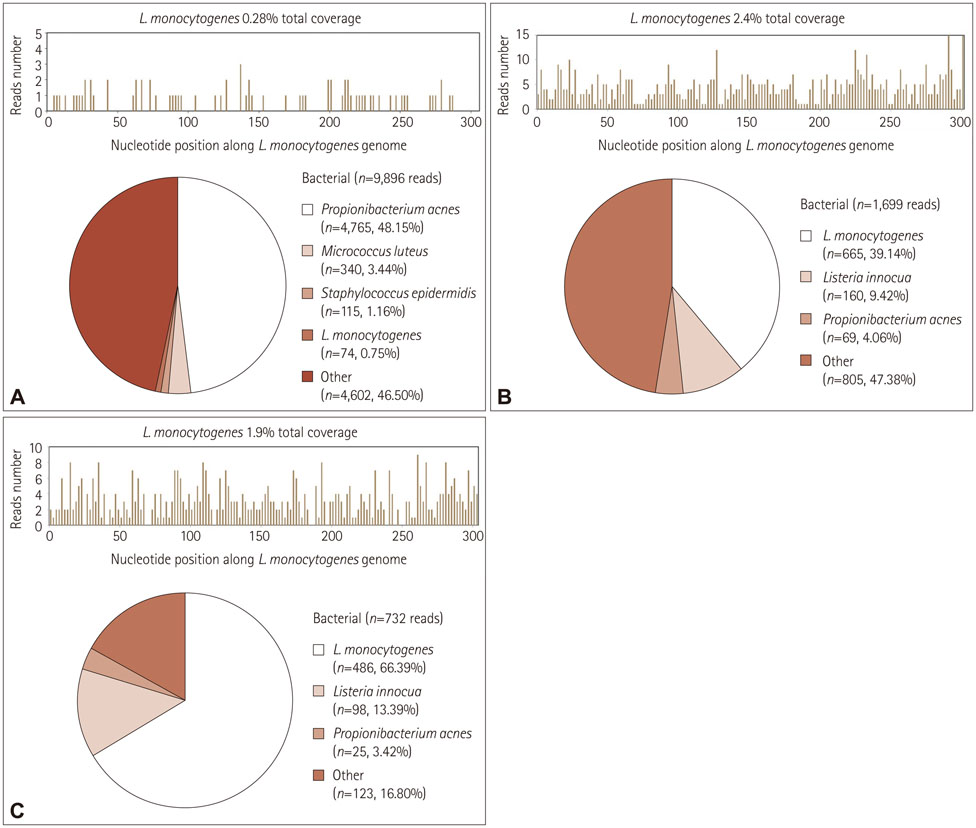
This study set up and applied unbiased NGS to detect L. monocytogenes in CSF collected from three cases of clinically suspected listeria meningoencephalitis.
RESULTS
Three cases of patients with acute/subacute meningoencephalitis are reported. Magnetic resonance imaging and blood cultures led to a suspected diagnosis of L. monocytogenes, while the CSF cultures were negative. Unbiased NGS of CSF identified and sequenced reads corresponding to L. monocytogenes in all three cases.
CONCLUSIONS
This is the first report highlighting the feasibility of applying NGS of CSF as a diagnostic method for central nervous system (CNS) L. monocytogenes infection. Routine application of this technology in clinical microbiology will significantly improve diagnostic methods for CNS infectious diseases.
Keyword
MeSH Terms
Figure
Reference
-
1. Workman S, Theal M. Rhomboencephalitis caused by Listeria monocytogenes. Can J Infect Dis. 1997; 8:113–116.2. Armstrong RW, Fung PC. Brainstem encephalitis (rhombencephalitis) due to Listeria monocytogenes: case report and review. Clin Infect Dis. 1993; 16:689–702.
Article3. Mylonakis E, Hohmann EL, Calderwood SB. Central nervous system infection with Listeria monocytogenes. 33 years' experience at a general hospital and review of 776 episodes from the literature. Medicine (Baltimore). 1998; 77:313–336.
Article4. Paul ML, Dwyer DE, Chow C, Robson J, Chambers I, Eagles G, et al. Listeriosis--a review of eighty-four cases. Med J Aust. 1994; 160:489–493.5. Long SW, Williams D, Valson C, Cantu CC, Cernoch P, Musser JM, et al. A genomic day in the life of a clinical microbiology laboratory. J Clin Microbiol. 2013; 51:1272–1277.
Article6. Grard G, Fair JN, Lee D, Slikas E, Steffen I, Muyembe JJ, et al. A novel rhabdovirus associated with acute hemorrhagic fever in central Africa. PLoS Pathog. 2012; 8:e1002924.
Article7. Wilson MR, Naccache SN, Samayoa E, Biagtan M, Bashir H, Yu G, et al. Actionable diagnosis of neuroleptospirosis by next-generation sequencing. N Engl J Med. 2014; 370:2408–2417.
Article8. Briese T, Paweska JT, McMullan LK, Hutchison SK, Street C, Palacios G, et al. Genetic detection and characterization of Lujo virus, a new hemorrhagic fever-associated arenavirus from southern Africa. PLoS Pathog. 2009; 5:e1000455.
Article9. Yu G, Greninger AL, Isa P, Phan TG, Martínez MA, de la Luz Sanchez M, et al. Discovery of a novel polyomavirus in acute diarrheal samples from children. PLoS One. 2012; 7:e49449.
Article10. Jeon YJ, Zhou Y, Li Y, Guo Q, Chen J, Quan S, et al. The feasibility study of non-invasive fetal trisomy 18 and 21 detection with semiconductor sequencing platform. PLoS One. 2014; 9:e110240.
Article11. Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009; 25:1754–1760.
Article12. Reynaud L, Graf M, Gentile I, Cerini R, Ciampi R, Noce S, et al. A rare case of brainstem encephalitis by Listeria monocytogenes with isolated mesencephalic localization. Case report and review. Diagn Microbiol Infect Dis. 2007; 58:121–123.
Article13. Cunha BA, Fatehpuria R, Eisenstein LE. Listeria monocytogenes encephalitis mimicking Herpes Simplex virus encephalitis: the differential diagnostic importance of cerebrospinal fluid lactic acid levels. Heart Lung. 2007; 36:226–231.
Article14. Fournier PE, Dubourg G, Raoult D. Clinical detection and characterization of bacterial pathogens in the genomics era. Genome Med. 2014; 6:114.
Article15. Sherry NL, Porter JL, Seemann T, Watkins A, Stinear TP, Howden BP. Outbreak investigation using high-throughput genome sequencing within a diagnostic microbiology laboratory. J Clin Microbiol. 2013; 51:1396–1401.
Article16. Padmanabhan R, Mishra AK, Raoult D, Fournier PE. Genomics and metagenomics in medical microbiology. J Microbiol Methods. 2013; 95:415–424.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple, Diffuse Brain Abscesses due to Listeria Monocytogenes
- A case of meningoencephalitis caused by Listeria monocytogenes in a healthy child
- A Case of Listeria Meningoencephalitis in a Healthy Child
- Liver Abscess Caused by Listeria monocytogenes : A Case Report
- Species-Specific Detection of Listeria monocytogenes by Polymerase Chain Reaction