J Korean Assoc Oral Maxillofac Surg.
2017 Feb;43(1):46-48. 10.5125/jkaoms.2017.43.1.46.
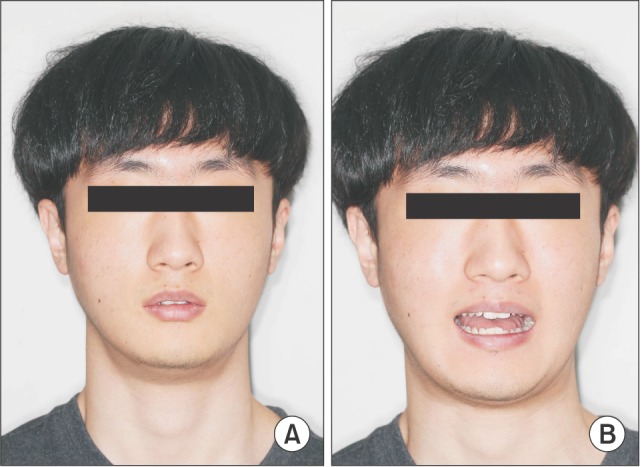
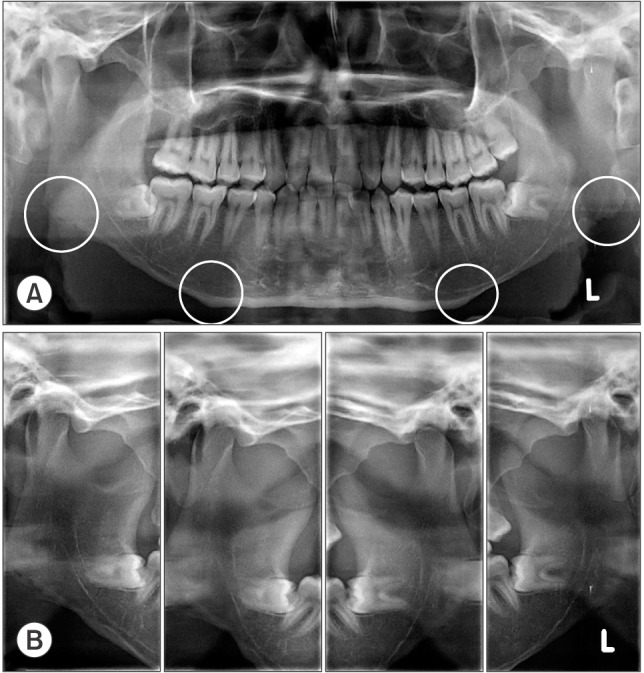
The postoperative trismus, nerve injury and secondary angle formation after partial masseter muscle resection combined with mandibular angle reduction: a case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Section of Dentistry, SMG-SNU Boramae Medical Center, Seoul, Korea. hanomfs@gmail.com
- 2Department of Oral and Maxillofacial Surgery, School of Dentistry, Seoul National University, Seoul, Korea.
- KMID: 2385070
- DOI: http://doi.org/10.5125/jkaoms.2017.43.1.46
Abstract
- A patient, who underwent partial masseter muscle resection and mandibular angle reduction at a plastic surgery clinic, visited this hospital with major complaints of trismus and dysesthesia. A secondary angle formation due to a wrong surgical method was observed via clinical and radiological examinations, and the patient complained of trismus due to the postoperative scars and muscular atrophy caused by the masseter muscle resection. The need for a masseter muscle resection in square jaw patients must be approached with caution. In addition, surgical techniques must be carefully selected in order to prevent complications, and obtain effective and satisfactory surgery results.
Keyword
MeSH Terms
Figure
Reference
-
1. Baek SM, Kim SS, Bindiger A. The prominent mandibular angle: preoperative management, operative technique, and results in 42 patients. Plast Reconstr Surg. 1989; 83:272–280. PMID: 2911627.2. Yang DB, Song HS, Park CG. Unfavorable results and their resolution in mandibular contouring surgery. Aesthetic Plast Surg. 1995; 19:93–102. PMID: 7900562.
Article3. Baek SM, Baek RM, Shin MS. Refinement in aesthetic contouring of the prominent mandibular angle. Aesthetic Plast Surg. 1994; 18:283–289. PMID: 7976763.
Article4. Yoon ES, Seo YS, Kang DH, Koo SH, Park SH. Analysis of incidences and types of complications in mandibular angle ostectomy in Koreans. Ann Plast Surg. 2006; 57:541–544. PMID: 17060736.
Article5. Min L, Lai G, Xin L. Changes in masseter muscle following curved ostectomy of the prominent mandibular angle: an initial study with real-time 3D ultrasonograpy. J Oral Maxillofac Surg. 2008; 66:2434–2443. PMID: 19022120.
Article6. Pary A, Pary K. Masseteric hypertrophy: considerations regarding treatment planning decisions and introduction of a novel surgical technique. J Oral Maxillofac Surg. 2011; 69:944–949. PMID: 21195532.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experience of External Carotid A-V Fistula after Reduction Mandibuloplasty
- Surgical correction of masseter muscle hypertrophy: report of three cases
- Introduction of Radiofrequency Reduction of Masseter Muscle and Case Reports
- Surgical Correction of Squared Mandibular Face
- Mandibular Angle Reduction By Selective Extraoral Approach