J Korean Assoc Oral Maxillofac Surg.
2017 Feb;43(1):23-28. 10.5125/jkaoms.2017.43.1.23.
Comparative study of postoperative stability between conventional orthognathic surgery and a surgery-first orthognathic approach after bilateral sagittal split ramus osteotomy for skeletal class III correction
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Chosun University, Gwangju, Korea. sgckim@chosun.ac.kr
- KMID: 2385066
- DOI: http://doi.org/10.5125/jkaoms.2017.43.1.23
Abstract
OBJECTIVES
The purpose of this study is to compare the postoperative stability of conventional orthognathic surgery to a surgery-first orthognathic approach after bilateral sagittal split ramus osteotomy (BSSRO).
MATERIALS AND METHODS
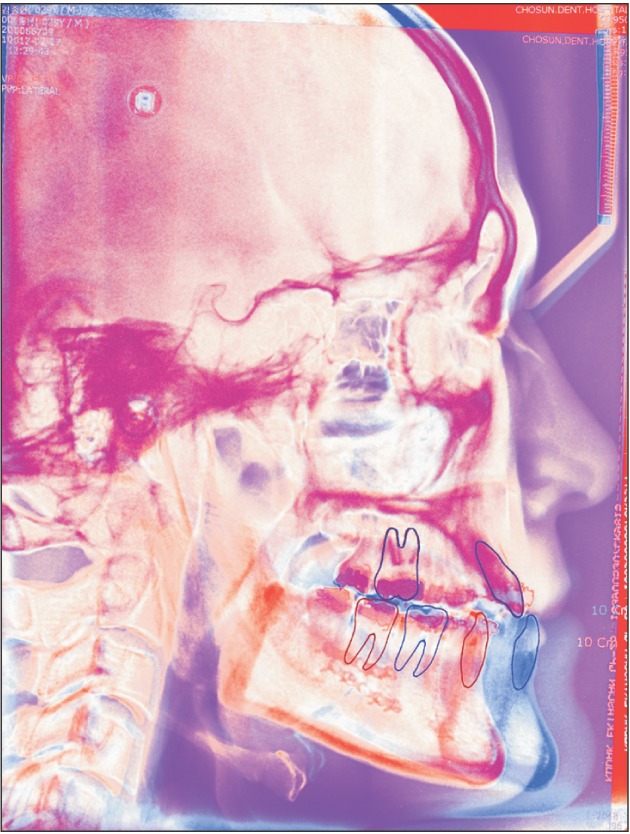
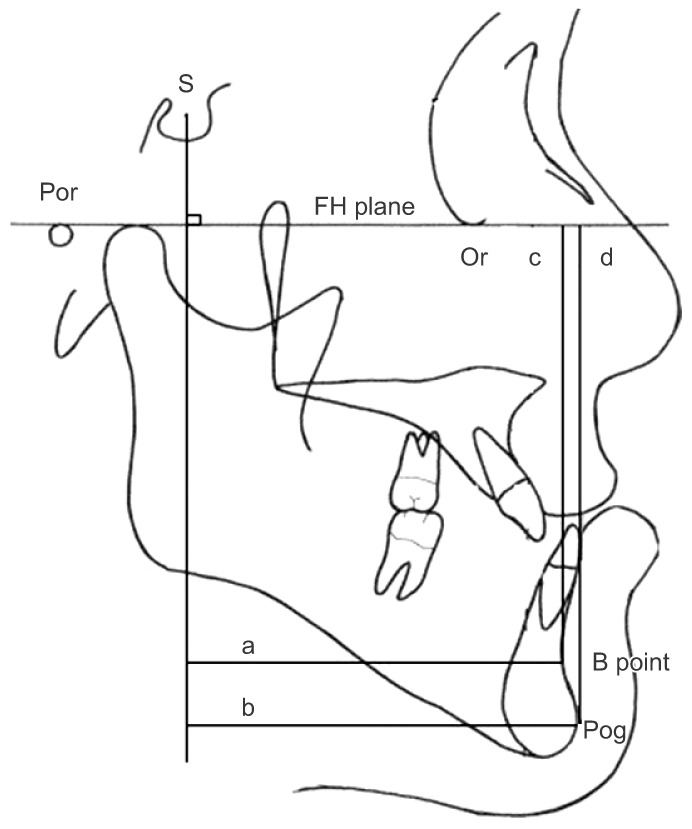
The study included 20 patients who underwent BSSRO for skeletal class III conventional orthognathic surgery and 20 patients who underwent a surgery-first orthognathic approach. Serial lateral cephalograms were analyzed to identify skeletal changes before surgery (T0), immediately after surgery (T1), and after surgery (T2, after 1 year or at debonding).
RESULTS
The amount of relapse of the mandible in the conventional orthognathic surgery group from T1 to T2 was 2.23±0.92 mm (P<0.01) forward movement and −0.87±0.57 mm (non-significant, NS) upward movement on the basis of point B and 2.54±1.37 mm (P<0.01) forward movement and −1.18±0.79 mm (NS) upward movement on the basis of the pogonion (Pog) point. The relapse amount of the mandible in the surgery-first orthognathic approach group from T1 to T2 was 3.49±1.71 mm (P<0.01) forward movement and −1.78±0.81 mm (P<0.01) upward movement on the basis of the point B and 4.11±1.93 mm (P<0.01) forward movement and −2.40±0.98 mm (P<0.01) upward movement on the basis of the Pog.
CONCLUSION
The greater horizontal and vertical relapse may appear because of counter-clockwise rotation of the mandible in surgery-first orthognathic approach. Therefore, careful planning and skeletal stability should be considered in orthognathic surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Kang HK, Ryu YK. A study on the prevalence of malocclusion of Yonsei university students in 1991. Korean J Orthod. 1992; 22:691–701.2. Baik HS, Han HK, Kim DJ, Proffit WR. Cephalometric characteristics of Korean Class III surgical patients and their relationship to plans for surgical treatment. Int J Adult Orthodon Orthognath Surg. 2000; 15:119–128. PMID: 11307422.3. Bos A, Hoogstraten J, Prahl-Andersen B. Expectations of treatment and satisfaction with dentofacial appearance in orthodontic patients. Am J Orthod Dentofacial Orthop. 2003; 123:127–132. PMID: 12594417.
Article4. Juggins KJ, Nixon F, Cunningham SJ. Patient- and clinician-perceived need for orthognathic surgery. Am J Orthod Dentofacial Orthop. 2005; 128:697–702. PMID: 16360908.
Article5. Dowling PA, Espeland L, Krogstad O, Stenvik A, Kelly A. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:146–152. PMID: 10686838.6. Luther F, Morris DO, Hart C. Orthodontic preparation for orthognathic surgery: how long does it take and why? A retrospective study. Br J Oral Maxillofac Surg. 2003; 41:401–406. PMID: 14614870.
Article7. Proffit WR, White RP, Sarver DM. Contemporary treatment of dentofacial deformity. St. Louis: Mosby;2003.8. Nagasaka H, Sugawara J, Kawamura H, Nanda R. “Surgery first” skeletal Class III correction using the Skeletal Anchorage System. J Clin Orthod. 2009; 43:97–105. PMID: 19276579.9. Baek SH, Ahn HW, Kwon YH, Choi JY. Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: evaluation of surgical movement and postoperative orthodontic treatment. J Craniofac Surg. 2010; 21:332–338. PMID: 20186090.10. Yu CC, Chen PH, Liou EJ, Huang CS, Chen YR. A surgery-first approach in surgical-orthodontic treatment of mandibular prognathism--a case report. Chang Gung Med J. 2010; 33:699–705. PMID: 21199616.11. Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994; 65:79–83. PMID: 8133418.
Article12. Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg. 2011; 69:781–785. PMID: 21353934.
Article13. Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957; 10:677–689. PMID: 13441284.14. Dal Pont G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anesth Hosp Dent Serv. 1961; 19:42–47. PMID: 13719390.15. de Villa GH, Huang CS, Chen PK, Chen YR. Bilateral sagittal split osteotomy for correction of mandibular prognathism: long-term results. J Oral Maxillofac Surg. 2005; 63:1584–1592. PMID: 16243174.
Article16. Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996; 11:191–204. PMID: 9456622.17. Villegas C, Uribe F, Sugawara J, Nanda R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010; 44:97–103. PMID: 20552809.18. Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: orthodontic guidelines and setup for model surgery. J Oral Maxillofac Surg. 2011; 69:771–780. PMID: 21257249.
Article19. Bailey L, Cevidanes LH, Proffit WR. Stability and predictability of orthognathic surgery. Am J Orthod Dentofacial Orthop. 2004; 126:273–277. PMID: 15356484.
Article20. Jacobs JD, Sinclair PM. Principles of orthodontic mechanics in orthognathic surgery cases. Am J Orthod. 1983; 84:399–407. PMID: 6579841.
Article21. Costa F, Robiony M, Politi M. Stability of sagittal split ramus osteotomy used to correct Class III malocclusion: review of the literature. Int J Adult Orthodon Orthognath Surg. 2001; 16:121–129. PMID: 11482290.22. Ko EW, Lin SC, Chen YR, Huang CS. Skeletal and dental variables related to the stability of orthognathic surgery in skeletal Class III malocclusion with a surgery-first approach. J Oral Maxillofac Surg. 2013; 71:e215–e223. PMID: 23455415.
Article23. Downs WB. Variations in facial relationships; their significance in treatment and prognosis. Am J Orthod. 1948; 34:812–840. PMID: 18882558.
Article24. Burstone CJ, James RB, Legan H, Murphy GA, Norton LA. Cephalometrics for orthognathic surgery. J Oral Surg. 1978; 36:269–277. PMID: 273073.25. Kim JH, Mahdavie NN, Evans CA. Guidelines for “Surgery First” orthodontic treatment. In : Bourzgui F, editor. Orthodontics: basic aspects and clinical considerations. Rijeka, Croatia: InTech;2012. p. 265–300.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two treatment approach to skeletal Class III : A case report on sisters
- The study of the soft tissue change according to skeletal change following bssro with advancing genioplasty
- Comparative study on long-term stability in mandibular sagittal split ramus osteotomy: hydroxyapatite/poly-l-lactide mesh versus titanium miniplate
- Horner's Syndrome after Orthognathic Surgery
- Stability of orthognathic surgery for cleft lip and palate patients