Ann Rehabil Med.
2012 Dec;36(6):861-865.
Dysphagia due to Retropharyngeal Abscess that Incidentally Detected in Subarachnoid Hemorrhage Patient
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, College of Medicine, Dongguk University, Goyang 410-773, Korea. jinwoo.park.md@gmail.com
Abstract
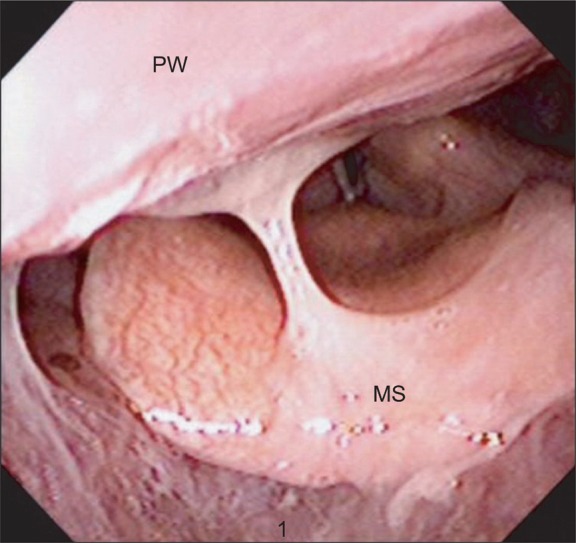
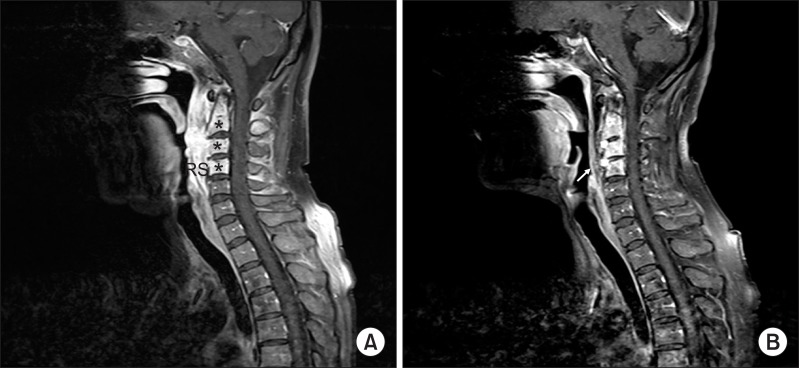
- Cerebral hemorrhage is one of the most common causes of dysphagia. In many cases, dysphagia gets better once the acute phase has passed. Structural lesions such as thyromegaly, cervical hyperostosis, congenital web, Zenker's diverticulum, neoplasm, radiation fibrosis, and retropharyngeal abscess must be considered as other causes of dysphagia as well. Retropharyngeal abscess seldom occur in adults and if it does so, a search for a prior dental procedure, trauma, head and neck infection is needed. The symptoms may include neck pain, dysphagia, sore throat, and in rare cases, dyspnea accompanied by stridor. We present a case and discuss a patient who had dysphagia and neck pain after a cerebral hemorrhage. Testing revealed a retropharyngeal abscess. The symptoms were successfully treated after the administration of antibiotics.
Keyword
MeSH Terms
Figure
Reference
-
1. Braddom RL. Physical medicine & rehabilitation. 2011. 4th ed. Philadelphia: Elsevier Inc;p. 584–588.2. Han TR, Bang MS. Rehabilitation medicine. 2008. 3rd ed. Seoul: Koonja;p. 375–379.3. Veis SL, Logemann JA. Swallowing disorders in persons with cerebrovascular accident. Arch Phys Med Rehabil. 1985; 66:372–375. PMID: 4004534.4. Martino R, Terrault N, Ezerzer F, Mikulis D, Diamant NE. Dysphagia in a patient with lateral medullary syndrome: insight into the central control of swallowing. Gastroenterology. 2001; 121:420–426. PMID: 11487551.
Article6. Coulthard M, Isaacs D. Retropharyngeal abscess. Arch Dis Child. 1991; 66:1227–1230. PMID: 1953008.
Article7. Tannebaum RD. Adult retropharyngeal abscess: a case report and review of literature. J Emerg Med. 1996; 14:147–158. PMID: 8740744.8. Crury MA, Groher ME. Introduction to adult swallowing disorders. 2003. Florida: Elsevier Inc;p. 1–49.9. Karkanevatos A, Beasley NJ, Swift AC. Acute non-tuberculous retropharyngeal abscess in an adult. A case report and review of the literature. J Laryngol Otol. 1997; 111:169–171. PMID: 9102447.
Article10. Rotta AT, Wiryawan B. Respiratory emergencies in children. Respir Care. 2003; 48:248–258. PMID: 12667275.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dysphagia after Retropharyngeal Abscess Treated with Transcutaneous Injection of Botulinum Toxin at Cricopharyngeus Muscle
- A Case of Second Branchial Cyst in Retropharyngeal Space, Appearing as Dyspnea and Dysphagia
- Intramural Esophageal Abscess and Dissection due to Retropharygeal Abscess
- A Case of Retropharyngeal Abscess and Mediastinal Abscess with Dyspnea
- Retropharyngeal Abscess Associated with Osteomyelitis of the Cervical Spine and an Epidural Abscess