Korean J Ophthalmol.
2017 Jun;31(3):277-279. 10.3341/kjo.2017.0004.
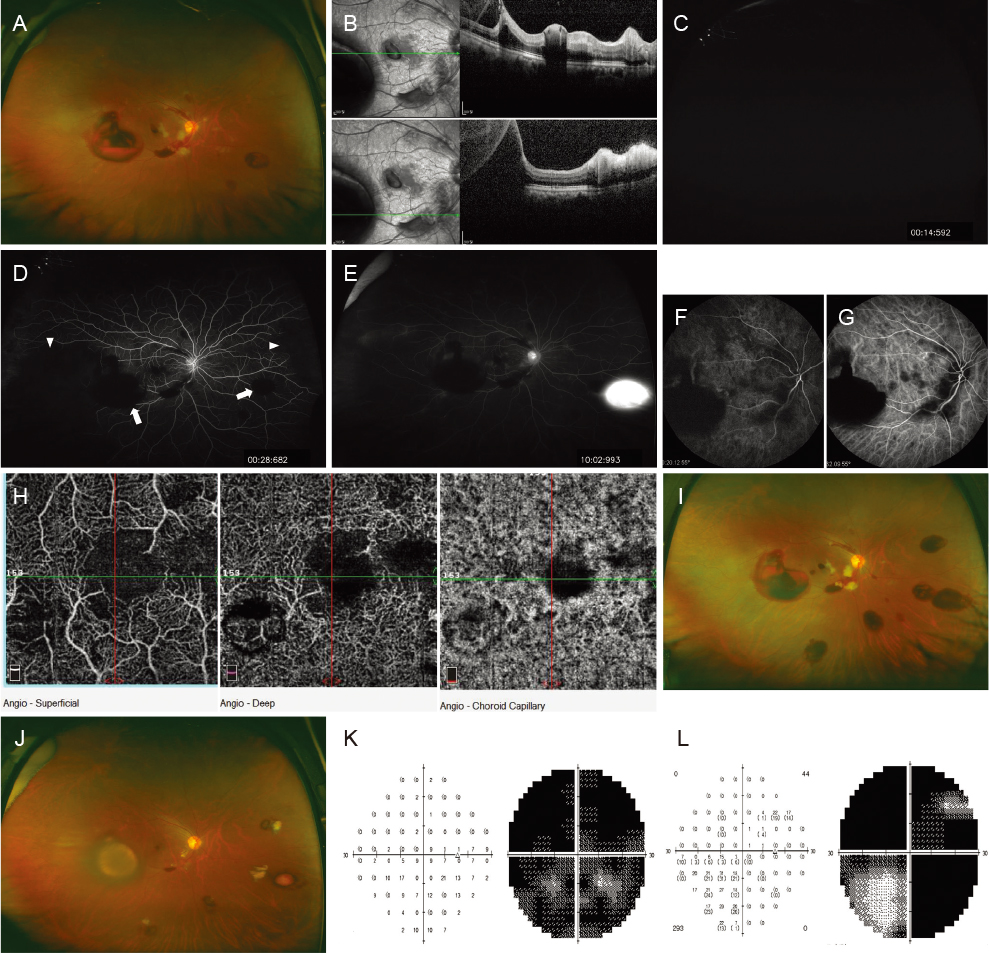
A Case of Ophthalmic Artery Occlusion Following Subcutaneous Injection of Epinephrine Mixed with Lidocaine into the Supratrochlear Area
- Affiliations
-
- 1Retina Center, Department of Ophthalmology, HanGil Eye Hospital, Incheon, Korea.
- 2Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. junekim@amc.seoul.kr
- KMID: 2379886
- DOI: http://doi.org/10.3341/kjo.2017.0004
Abstract
- No abstract available.
Figure
Reference
-
1. Niemi G. Advantages and disadvantages of adrenaline in regional anaesthesia. Best Pract Res Clin Anaesthesiol. 2005; 19:229–245.2. Park KH, Kim YK, Woo SJ, et al. Iatrogenic occlusion of the ophthalmic artery after cosmetic facial filler injections: a national survey by the Korean Retina Society. JAMA Ophthalmol. 2014; 132:714–723.3. Lazzeri D, Agostini T, Figus M, et al. Blindness following cosmetic injections of the face. Plast Reconstr Surg. 2012; 129:995–1012.4. Savino PJ, Burde RM, Mills RP. Visual loss following intranasal anesthetic injection. J Clin Neuroophthalmol. 1990; 10:140–144.5. Webber B, Orlansky H, Lipton C, Stevens M. Complications of an intra-arterial injection from an inferior alveolar nerve block. J Am Dent Assoc. 2001; 132:1702–1704.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Teh Effect of Local anesthetic on Degeneration and Regeneration of the Experimentally Traumatized Striated Muscle
- A Case of Unilateral Blindness Following Subcutaneous Injection of the silicone Oil on the Glabellar Area
- The Antimicrobial effects of Lidocaine and Epinephrine
- Effects of Epinephrine on Blood Concentration of Lidocaine and Epidural Block during Cesarean Section
- Ophthalmic Artery Occlusion After Carotid Revascularization