J Menopausal Med.
2016 Dec;22(3):180-183. 10.6118/jmm.2016.22.3.180.
Superficial Angiomyxoma of the Vulva in a Postmenopausal Woman: A Case Report and Review of Literature
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Dong-A University College of Medicine, Busan, Korea. jeanjane@naver.com
- 2Department of Pathology, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2378239
- DOI: http://doi.org/10.6118/jmm.2016.22.3.180
Abstract
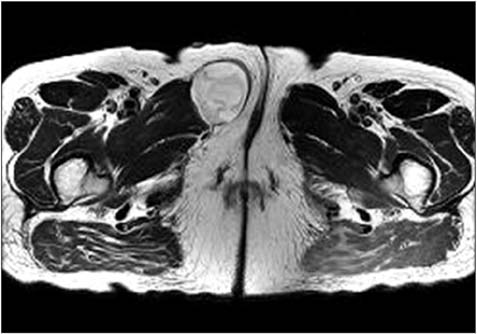
- Superficial angiomyxomas (SAMs) are rare benign cutaneous tumors that involve the subcutaneous layer. They are commonly located in the trunk, lower limbs and head or neck of women of reproductive age. SAMs in the vulva of postmenopausal women are especially rare case. Herein, we report a vulvar SAM in a postmenopausal 60-year-old woman. The patient presented with a palpable cutaneous mass in the right labium majora that had appeared 3 months earlier. The mass was slow growing and approximately 5 cm in size and resembled a soft tissue malignancy. It appeared as a well-defined multilocular cystic mass in magnetic resonance images. The preoperative diagnosis was a benign cystic lesion such as an epidermoid cyst. Grossly, the completely excised mass was 6 × 5 cm in size and well circumscribed with a multilocular outer surface, a yellowish-gray gelatinous cut surface, and a smooth rubbery inner surface. Histologic review revealed that the mass contained small to moderate amount of cellular angiomyxoid nodules and bland-looking spindle-shaped to ovoid cells without atypia. Neutrophil infiltration, which is a diagnostic feature of SAMs, was observed. Immunohistochemistry showed expression of CD34, but not of estrogen receptors, progesterone receptors, or desmin in the SAM. The patient has been followed up for 12 months without recurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Carney JA, Headington JT, Su WP. Cutaneous myxomas. A major component of the complex of myxomas, spotty pigmentation, and endocrine overactivity. Arch Dermatol. 1986; 122:790–798.2. Allen PW. Myxoma is not a single entity: a review of the concept of myxoma. Ann Diagn Pathol. 2000; 4:99–123.3. Allen PW, Dymock RB, MacCormac LB. Superficial angiomyxomas with and without epithelial components. Report of 30 tumors in 28 patients. Am J Surg Pathol. 1988; 12:519–530.4. Fetsch JF, Laskin WB, Tavassoli FA. Superficial angiomyxoma (cutaneous myxoma): a clinicopathologic study of 17 cases arising in the genital region. Int J Gynecol Pathol. 1997; 16:325–334.5. Calonje E, Guerin D, McCormick D, Fletcher CD. Superficial angiomyxoma: clinicopathologic analysis of a series of distinctive but poorly recognized cutaneous tumors with tendency for recurrence. Am J Surg Pathol. 1999; 23:910–917.6. Kim TH, Lee HH, Chung SH, Hwang IC, Han HS. Fibroepithelial polyps on an unusual genital site during menopausal transition. J Korean Soc Menopause. 2011; 17:110–113.7. Nucci MR, Fletcher CD. Vulvovaginal soft tissue tumours: update and review. Histopathology. 2000; 36:97–108.8. Kim HS, Kim GY, Lim SJ, Ki KD, Kim HC. Giant superficial angiomyxoma of the vulva: a case report and review of the literature. J Cutan Pathol. 2010; 37:672–677.9. Metin A, Nese CD, Nagihan C, Ender D. Aggressive angiomyxoma of the vulva: a case report and review of the literature. Aegean Pathol J. 2006; 3:1–4.10. Kura MM, Jindal SR, Khemani UN. Aggressive angiomyxoma of the vulva: An uncommon entity. Indian Dermatol Online J. 2012; 3:128–130.11. Blandamura S, Cruz J, Faure Vergara L, Machado Puerto I, Ninfo V. Aggressive angiomyxoma: a second case of metastasis with patient's death. Hum Pathol. 2003; 34:1072–1074.12. Fetsch JF, Laskin WB, Lefkowitz M, Kindblom LG, Meis-Kindblom JM. Aggressive angiomyxoma: a clinicopathologic study of 29 female patients. Cancer. 1996; 78:79–90.