J Clin Neurol.
2017 Apr;13(2):196-198. 10.3988/jcn.2017.13.2.196.
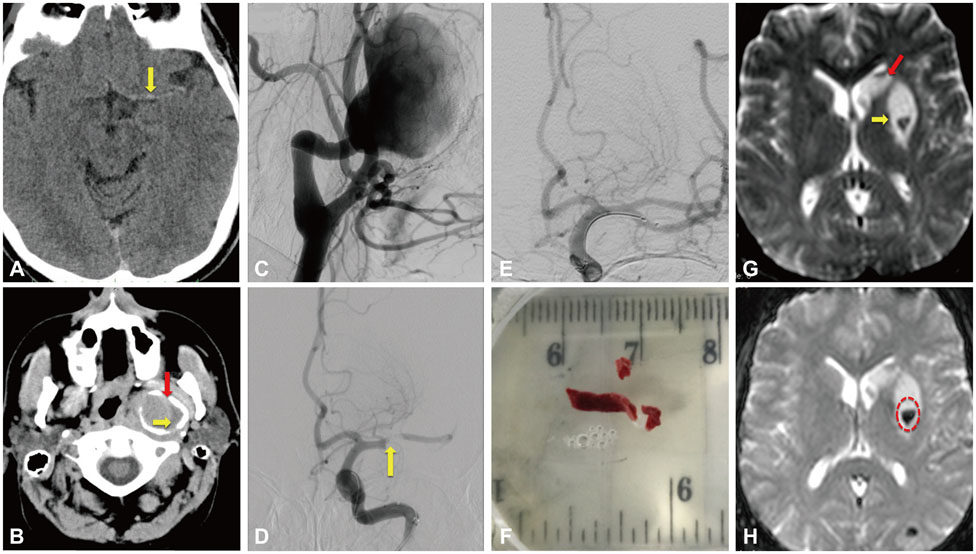
Mechanical Thrombectomy for Acute Middle Cerebral Artery Occlusion Caused by a Giant, Thrombosed, Extracranial Internal Carotid Artery Aneurysm
- Affiliations
-
- 1Stroke Unit, Metropolitan Hospital, Piraeus, Greece.
- 2Stroke Unit, Department of Neurology, Brugmann University Hospital, Bruxelles, Belgium.
- 3Second Department of Neurology, "Attikon" Hospital, School of Medicine, University of Athens, Athens, Greece. tsivgoulisgiorg@yahoo.gr
- 4Department of Neurology, School of Medicine, University of Ioannina, Ioannina, Greece.
- 5Department of Neurology, The University of Tennessee Health Science Center, Memphis, Tennessee, United States of America.
- 6Department of Neurology, International Clinical Research Center, St. Anne's University Hospital in Brno, Brno, Czech Republic.
- KMID: 2376022
- DOI: http://doi.org/10.3988/jcn.2017.13.2.196
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients With acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035.
Article2. Campbell BC, Donnan GA, Lees KR, Hacke W, Khatri P, Hill MD, et al. Endovascular stent thrombectomy: the new standard of care for large vessel ischaemic stroke. Lancet Neurol. 2015; 14:846–854.
Article3. Fields JD, Lutsep HL, Rymer MR, Budzik RF, Devlin TG, Baxter BW, et al. Endovascular mechanical thrombectomy for the treatment of acute ischemic stroke due to arterial dissection. Interv Neuroradiol. 2012; 18:74–79.
Article4. Zibold F, Kleine JF, Zimmer C, Poppert H, Boeckh-Behrens T. Aneurysms in the target vessels of stroke patients subjected to mechanical thrombectomy: prevalence and impact on treatment. J Neurointerv Surg. 2016; 8:1016–1020.
Article5. Bhole R, Goyal N, Nearing K, Belayev A, Doss VT, Elijovich L, et al. Implications of limiting mechanical thrombectomy to patients with emergent large vessel occlusion meeting top tier evidence criteria. J Neurointerv Surg. 2016; 03. 1. [Epub]. DOI: 10.1136/neurintsurg-2015-012206.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to Escape Stentriever Wedging in an Open-cell Carotid Stent during Mechanical Thrombectomy for Tandem Cervical Internal Carotid Artery and Middle Cerebral Artery Occlusion
- Aneurysmectomy and graft interposition for giant thrombosed proximal internal carotid artery aneurysm: Technical details
- Aspiration Clot Removal by Mannual Compression of Common Carotid Artery for Acute Internal Carotid Occlusion: a Case Report
- Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: A literature review
- Completely Thrombosed Contralateral Internal Carotid Artery Aneurysm Combined with Ruptured Anterior Communicating Artery Aneurysm: Case Report