J Dent Anesth Pain Med.
2017 Mar;17(1):55-59. 10.17245/jdapm.2017.17.1.55.
Creating protective appliances for preventing dental injury during endotracheal intubation using intraoral scanning and 3D printing: a technical note
- Affiliations
-
- 1Department of Advanced General Dentistry, College of Dentistry, Yonsei University, Seoul, Korea. kdkim@yuhs.ac
- KMID: 2374724
- DOI: http://doi.org/10.17245/jdapm.2017.17.1.55
Abstract
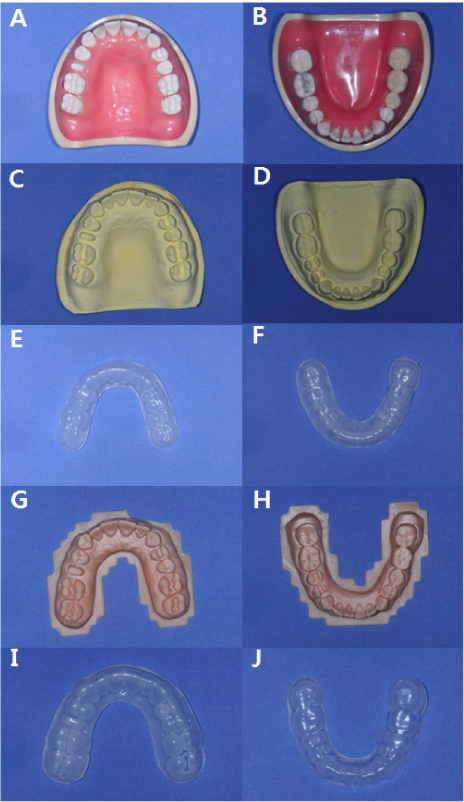
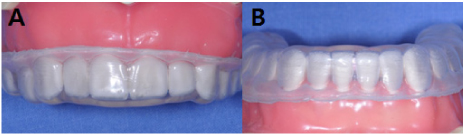
- Digital dentistry has influenced many dental procedures, such as three-dimensional (3D) diagnosis and treatment planning, surgical splints, and prosthetic treatments. Patient-specific protective appliances (PSPAs) prevent dental injury during endotracheal intubation. However, the required laboratory work takes time, and there is the possibility of tooth extraction while obtaining the dental impression. In this technical report, we utilized new digital technology for creating PSPAs, using direct intraoral scanners and 3D printers for dental cast fabrication.
Keyword
MeSH Terms
Figure
Reference
-
1. Chen JJ, Susetio L, Chao CC. Oral complications associated with endotracheal general anesthesia. Ma Zui Xue Za Zhi. 1990; 28:163–169.2. Lockhart PB, Feldbau EV, Gabel RA, Connolly SF, Silversin JB. Dental complications during and after tracheal intubation. J Am Dent Assoc. 1986; 112:480–483.
Article3. Burton JF, Baker AB. Dental damage during anaesthesia and surgery. Anaesth Intensive Care. 1987; 15:262–268.
Article4. Deppe H, Reeker W, Horch HH, Kochs E. Tooth injury during intubation--diagnostic and therapeutic aspects. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998; 33:722–725.5. Ghabash MB, Matta MS, Mehanna CB. Prevention of dental trauma during endotracheal intubation. Anesth Analg. 1997; 84:230–231.
Article6. Lee KH, You TM, Park W, Lee SH, Jung BY, Pang NS, et al. Protective dental splint for oroendotracheal intubation: Experience of 202 cases. J Dent Anesth Pain Med. 2015; 15:17–23.
Article7. Akyalcin S, Cozad BE, English JD, Colville CD, Laman S. Diagnostic accuracy of impression-free digital models. Am J Orthod Dentofacial Orthop. 2013; 144:916–922.
Article8. Nedelcu RG, Persson AS. Scanning accuracy and precision in 4 intraoral scanners: An in vitro comparison based on 3-dimensional analysis. J Prosthet Dent. 2014; 112:1461–1471.
Article9. De Luca Canto G, Pacheco-Pereira C, Lagravere MO, Flores-Mir C, Major PW. Intra-arch dimensional measurement validity of laser-scanned digital dental models compared with the original plaster models: A systematic review. Orthod Craniofac Res. 2015; 18:65–76.
Article10. Renne W, Ludlow M, Fryml J, Schurch Z, Mennito A, Kessler R, et al. Evaluation of the accuracy of 7 digital scanners: An in vitro analysis based on 3-dimensional comparisons. J Prosthet Dent. 2016.11. Mangano F, Shibli JA, Fortin T. Digital dentistry: New materials and techniques. Int J Dent. 2016; 2016:5261247.
Article12. Patzelt SB, Lamprinos C, Stampf S, Att W. The time efficiency of intraoral scanners: An in vitro comparative study. J Am Dent Assoc. 2014; 145:542–551.13. Chia HN, Wu BM. Recent advances in 3D printing of biomaterials. J Biol Eng. 2015; 9:4.
Article14. Kloeg EF, Collys K. Materials for mouth protectors. Rev Belge Med Dent (1984). 2003; 58:21–33.15. Manka-Malara K, Gawlak D, Hovhannisyan A, Klikowska M, Kostrzewa-Janicka J. Dental trauma prevention during endotracheal intubation--review of literature. Anaesthesiol Intensive Ther. 2015; 47:425–429.16. Monaca E, Fock N, Doehn M, Wappler F. The effectiveness of preformed tooth protectors during endotracheal intubation: An upper jaw model. Anesth Analg. 2007; 105:1326–1332.
Article17. Sato N, Shingu K. Another reason to choose the left molar approach of laryngoscopy: To spare the incisor teeth. Anesthesiology. 2002; 96:1279.
Article18. Haddy S. Protecting teeth during endotracheal intubation. Anesthesiology. 1989; 71:810–811.
Article19. Hagelsten JO, Marvitz L. Prevention of dental damage during anesthesia. Z Prakt Anasth. 1971; 6:195–205.20. Field JM. Dental injuries during general anaesthesia. Br Dent J. 1996; 181:11.
Article21. Newland MC, Ellis SJ, Peters KR, Simonson JA, Durham TM, Ullrich FA, et al. Dental injury associated with anesthesia: A report of 161,687 anesthetics given over 14 years. J Clin Anesth. 2007; 19:339–345.
Article22. Cass NM. Medicolegal claims against anaesthetists: A 20 year study. Anaesth Intensive Care. 2004; 32:47–58.
Article23. Owen H, Waddell-Smith I. Dental trauma associated with anaesthesia. Anaesth Intensive Care. 2000; 28:133–145.
Article24. Klionsky DJ, Abdelmohsen K, Abe A, Abedin MJ, Abeliovich H, Acevedo Arozena A, et al. Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy. 2016; 12:1–222.25. Warner ME, Benenfeld SM, Warner MA, Schroeder DR, Maxson PM. Perianesthetic dental injuries: Frequency, outcomes, and risk factors. Anesthesiology. 1999; 90:1302–1305.
Article26. Magnin C, Bory EN, Motin J. Tooth injuries during intubation: A new preventive device. Ann Fr Anesth Reanim. 1991; 10:171–174.27. Folwaczny M, Hickel R. Oro-dental injuries during intubation anesthesia. Anaesthesist. 1998; 47:707–731.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endotracheal intubation using a three-dimensional printed airway model in a patient with Pierre Robin sequence and a history of tracheostomy -a case report-
- Medical Applications of 3D Printing and Standardization Issues
- Three-Dimensional Printing Technology in Orthopedic Surgery
- Mechanical properties and biocompatibility of experimental 3D printing denture base resin
- Management of Detachment of Pilot Balloon During Intraoral Repositioning of the Submental Endotracheal Tube