Yonsei Med J.
2016 Sep;57(5):1243-1251. 10.3349/ymj.2016.57.5.1243.
Predictors of False-Negative Results from Percutaneous Transthoracic Fine-Needle Aspiration Biopsy: An Observational Study from a Retrospective Cohort
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. khuhz@yuhs.ac
- 2Department of Nuclear Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2374172
- DOI: http://doi.org/10.3349/ymj.2016.57.5.1243
Abstract
- PURPOSE
We investigated factors predictive of false-negative pulmonary lesions with nonspecific benign cytology results on percutaneous transthoracic fine-needle aspiration biopsy (FNAB).
MATERIALS AND METHODS
We included 222 pulmonary lesions that had a nonspecific benign result from percutaneous transthoracic FNAB between March 2005 and December 2012, and were confirmed by subsequent pathologic results or adequate clinical follow up over at least 2 years. Clinical, imaging, and biopsy procedure-related findings were compared between lesions with a final diagnosis of malignancy (false-negative) and lesions with a benign diagnosis (true-negative). Multivariate logistic regression analysis was performed to identify significant predictors of false-negatives.
RESULTS
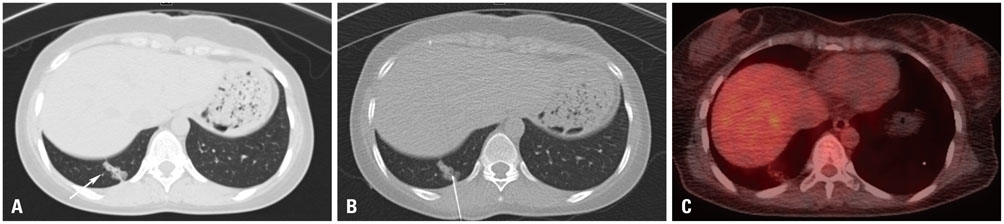
Of 222 lesions, 115 lesions were proved to be false-negatives, and 107 were true-negatives. Compared with the true-negatives, false-negative lesions showed significantly older age (p=0.037), higher maximum standardized uptake value (SUVmax) on positron emission tomography (p=0.001), larger lesion size (p=0.007), and lesion characteristics of a subsolid nodule (p=0.007). On multivariate logistic regression analysis, SUVmax, lesion size, and lesion characteristics were significant predictors of false-negative results.
CONCLUSION
Among the clinical, radiologic, and procedure-related factors analyzed, high SUVmax, large lesion size, and subsolid lesions were useful for predicting malignancy in pulmonary lesions with nonspecific benign cytology results on FNAB.
MeSH Terms
Figure
Cited by 1 articles
-
Study of the Efficacy of PET/CT in Lung Aspiration Biopsy and Factors Associated with False-Negative Results
Wan Son, Ji Won Lee, Yeon Joo Jeong, Ahrong Kim, Hie Bum Suh, Geewon Lee
J Korean Soc Radiol. 2018;79(3):129-138. doi: 10.3348/jksr.2018.79.3.129.
Reference
-
1. Tarver RD, Conces DJ Jr. Interventional chest radiology. Radiol Clin North Am. 1994; 32:689–709.2. Greif J, Marmor S, Schwarz Y, Staroselsky AN. Percutaneous core needle biopsy vs. fine needle aspiration in diagnosing benign lung lesions. Acta Cytol. 1999; 43:756–760.
Article3. Khouri NF, Stitik FP, Erozan YS, Gupta PK, Kim WS, Scott WW Jr, et al. Transthoracic needle aspiration biopsy of benign and malignant lung lesions. AJR Am J Roentgenol. 1985; 144:281–288.
Article4. Fraser RS. Transthoracic needle aspiration. The benign diagnosis. Arch Pathol Lab Med. 1991; 115:751–761.5. Stanley JH, Fish GD, Andriole JG, Gobien RP, Betsill WL, Laden SA, et al. Lung lesions: cytologic diagnosis by fine-needle biopsy. Radiology. 1987; 162:389–391.
Article6. Gelbman BD, Cham MD, Kim W, Libby DM, Smith JP, Port JL, et al. Radiographic and clinical characterization of false negative results from CT-guided needle biopsies of lung nodules. J Thorac Oncol. 2012; 7:815–820.
Article7. Savage C, Walser EM, Schnadig V, Woodside KJ, Ustuner E, Zwischenberger JB. Transthoracic image-guided biopsy of lung nodules: when is benign really benign? J Vasc Interv Radiol. 2004; 15(2 Pt 1):161–164.
Article8. Min JW, Lee SM, Chung DH, Yim JJ, Yang SC, Yoo CG, et al. Clinical significance of non-diagnostic pathology results from percutaneous transthoracic needle lung biopsy: experience of a tertiary hospital without an on-site cytopathologist. Respirology. 2009; 14:1042–1050.
Article9. Veale D, Gilmartin JJ, Sumerling MD, Wadehra V, Gibson GJ. Prospective evaluation of fine needle aspiration in the diagnosis of lung cancer. Thorax. 1988; 43:540–544.
Article10. Zakowski MF, Gatscha RM, Zaman MB. Negative predictive value of pulmonary fine needle aspiration cytology. Acta Cytol. 1992; 36:283–286.11. Molina R, Auge JM, Escudero JM, Marrades R, Viñolas N, Carcereny E, et al. Mucins CA 125, CA 19.9, CA 15.3 and TAG-72.3 as tumor markers in patients with lung cancer: comparison with CYFRA 21-1, CEA, SCC and NSE. Tumour Biol. 2008; 29:371–380.
Article12. Wieskopf B, Demangeat C, Purohit A, Stenger R, Gries P, Kreisman H, et al. Cyfra 21-1 as a biologic marker of non-small cell lung cancer. Evaluation of sensitivity, specificity, and prognostic role. Chest. 1995; 108:163–169.
Article13. Nestle U, Kremp S, Schaefer-Schuler A, Sebastian-Welsch C, Hellwig D, Rübe C, et al. Comparison of different methods for delineation of 18F-FDG PET-positive tissue for target volume definition in radiotherapy of patients with non-small cell lung cancer. J Nucl Med. 2005; 46:1342–1348.14. Priola AM, Priola SM, Cataldi A, Di Franco M, Pazè F, Marci V, et al. Diagnostic accuracy and complication rate of CT-guided fine needle aspiration biopsy of lung lesions: a study based on the experience of the cytopathologist. Acta Radiol. 2010; 51:527–533.
Article15. Ferran N, Ricart Y, Lopez M, Martinez-Ballarin I, Roca M, Gámez C, et al. Characterization of radiologically indeterminate lung lesions: 99mTc-depreotide SPECT versus 18F-FDG PET. Nucl Med Commun. 2006; 27:507–514.
Article16. Truong MT, Viswanathan C, Erasmus JJ. Positron emission tomography/computed tomography in lung cancer staging, prognosis, and assessment of therapeutic response. J Thorac Imaging. 2011; 26:132–146.
Article17. Shimizu K, Ikeda N, Tsuboi M, Hirano T, Kato H. Percutaneous CT-guided fine needle aspiration for lung cancer smaller than 2 cm and revealed by ground-glass opacity at CT. Lung Cancer. 2006; 51:173–179.
Article18. Minot DM, Gilman EA, Aubry MC, Voss JS, Van Epps SG, Tuve DJ, et al. An investigation into false-negative transthoracic fine needle aspiration and core biopsy specimens. Diagn Cytopathol. 2014; 42:1063–1068.
Article19. Lim HJ, Ahn S, Lee KS, Han J, Shim YM, Woo S, et al. Persistent pure ground-glass opacity lung nodules ≥ 10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest. 2013; 144:1291–1299.
Article20. Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology. 2013; 268:265–273.
Article21. Kim HY, Shim YM, Lee KS, Han J, Yi CA, Kim YK. Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology. 2007; 245:267–275.
Article22. Ohde Y, Nagai K, Yoshida J, Nishimura M, Takahashi K, Suzuki K, et al. The proportion of consolidation to ground-glass opacity on high resolution CT is a good predictor for distinguishing the population of non-invasive peripheral adenocarcinoma. Lung Cancer. 2003; 42:303–310.
Article23. Yanagawa M, Tanaka Y, Kusumoto M, Watanabe S, Tsuchiya R, Honda O, et al. Automated assessment of malignant degree of small peripheral adenocarcinomas using volumetric CT data: correlation with pathologic prognostic factors. Lung Cancer. 2010; 70:286–294.
Article24. Yanagawa M, Kuriyama K, Kunitomi Y, Tomiyama N, Honda O, Sumikawa H, et al. One-dimensional quantitative evaluation of peripheral lung adenocarcinoma with or without ground-glass opacity on thin-section CT images using profile curves. Br J Radiol. 2009; 82:532–540.
Article25. Matsuguma H, Yokoi K, Anraku M, Kondo T, Kamiyama Y, Mori K, et al. Proportion of ground-glass opacity on high-resolution computed tomography in clinical T1 N0 M0 adenocarcinoma of the lung: a predictor of lymph node metastasis. J Thorac Cardiovasc Surg. 2002; 124:278–284.
Article26. Higashiyama M, Kodama K, Yokouchi H, Takami K, Mano M, Kido S, et al. Prognostic value of bronchiolo-alveolar carcinoma component of small lung adenocarcinoma. Ann Thorac Surg. 1999; 68:2069–2073.
Article27. Sagawa M, Higashi K, Usuda K, Aikawa H, Machida Y, Tanaka M, et al. Curative wedge resection for non-invasive bronchioloalveolar carcinoma. Tohoku J Exp Med. 2009; 217:133–137.
Article28. Ikeda N, Maeda J, Yashima K, Tsuboi M, Kato H, Akada S, et al. A clinicopathological study of resected adenocarcinoma 2 cm or less in diameter. Ann Thorac Surg. 2004; 78:1011–1016.
Article29. Yoshida J, Nagai K, Yokose T, Nishimura M, Kakinuma R, Ohmatsu H, et al. Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg. 2005; 129:991–996.
Article30. Naidich DP, Bankier AA, MacMahon H, Schaefer-Prokop CM, Pistolesi M, Goo JM, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013; 266:304–317.
Article31. Laurent F, Latrabe V, Vergier B, Michel P. Percutaneous CT-guided biopsy of the lung: comparison between aspiration and automated cutting needles using a coaxial technique. Cardiovasc Intervent Radiol. 2000; 23:266–272.
Article32. Hong YJ, Hur J, Lee HJ, Nam JE, Kim YJ, Kim HS, et al. Analysis of tumor markers in the cytological fluid obtained from computed tomography-guided needle aspiration biopsy for the diagnosis of non-small cell lung cancer. J Thorac Oncol. 2011; 6:1330–1335.
Article33. Austin JH, Cohen MB. Value of having a cytopathologist present during percutaneous fine-needle aspiration biopsy of lung: report of 55 cancer patients and metaanalysis of the literature. AJR Am J Roentgenol. 1993; 160:175–177.
Article34. Padhani AR, Scott WW Jr, Cheema M, Kearney D, Erozan YS. The value of immediate cytologic evaluation for needle aspiration lung biopsy. Invest Radiol. 1997; 32:453–458.
Article35. Williams SM, Gray W, Gleeson FV. Macroscopic assessment of pulmonary fine needle aspiration biopsies: correlation with cytological diagnostic yield. Br J Radiol. 2002; 75:28–30.
Article36. Yamagami T, Iida S, Kato T, Tanaka O, Nishimura T. Combining fine-needle aspiration and core biopsy under CT fluoroscopy guidance: a better way to treat patients with lung nodules? AJR Am J Roentgenol. 2003; 180:811–815.
Article37. Beslic S, Zukic F, Milisic S. Percutaneous transthoracic CT guided biopsies of lung lesions; fine needle aspiration biopsy versus core biopsy. Radiol Oncol. 2012; 46:19–22.
Article38. Gong Y, Sneige N, Guo M, Hicks ME, Moran CA. Transthoracic fine-needle aspiration vs concurrent core needle biopsy in diagnosis of intrathoracic lesions: a retrospective comparison of diagnostic accuracy. Am J Clin Pathol. 2006; 125:438–444.
Article39. Choi SH, Chae EJ, Kim JE, Kim EY, Oh SY, Hwang HJ, et al. Percutaneous CT-guided aspiration and core biopsy of pulmonary nodules smaller than 1 cm: analysis of outcomes of 305 procedures from a tertiary referral center. AJR Am J Roentgenol. 2013; 201:964–970.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Fine Needle Aspiration Biopsy of Lung Masses
- Implantation Metastasis After Percutaneous Transthoracic Fine Needle Biopsy of Lung Cancer: A Case Report
- Cytopathologic Diagnosis of Pulmonary Diseases by Transthoracic Fine Needle Aspiration Biopsy
- Fine Needle Aspiration Biopsy Cytology of Breast Tumors
- Transthoracic Fine Needle Aspiration Biopsy: Diagnostic Rate and Complications in 1000 Cases