Yonsei Med J.
2016 Mar;57(2):430-440. 10.3349/ymj.2016.57.2.430.
Short-Term Analysis of Food Tolerance and Quality of Life after Laparoscopic Greater Curvature Plication
- Affiliations
-
- 1Department of Surgery, Gil Medical Center, Gachon University of Medicine and Science, Incheon, Korea. seongmin_kim@gilhospital.com
- KMID: 2374050
- DOI: http://doi.org/10.3349/ymj.2016.57.2.430
Abstract
- PURPOSE
The aim of this study was to compare short-term outcomes [food tolerance scores (FTS) and quality of life] after three types of restrictive bariatric surgery: laparoscopic adjustable gastric banding (LAGB), laparoscopic greater curvature plication (LGCP), and laparoscopic sleeve gastrectomy (LSG).
MATERIALS AND METHODS
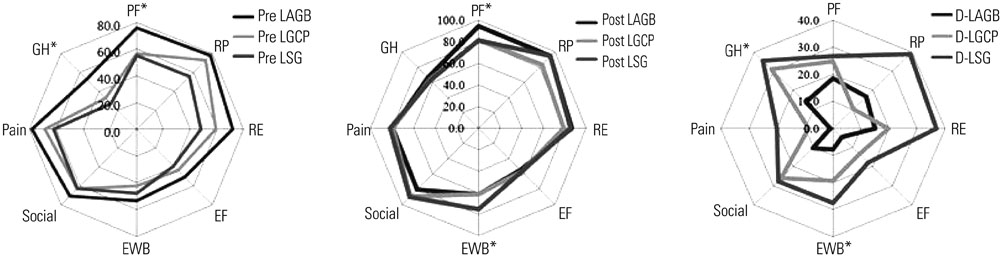
From January 2012 to December 2013, all patients that underwent primary surgery were included in one of the LAGB, LGCP, or LSG groups. These three groups were then compared with respect to FTS, gastrointestinal quality of life indices (GIQLI), and the Medical Outcomes Study Short-Form 36 (SF-36) questionnaire. Questionnaires were sent to all patients both pre- and post-operatively.
RESULTS
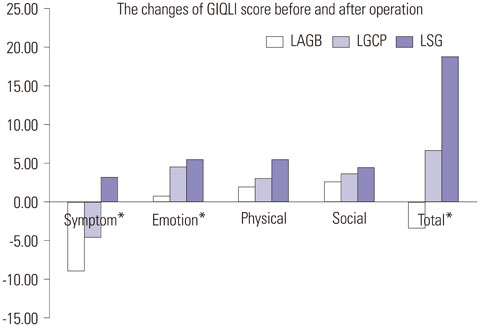
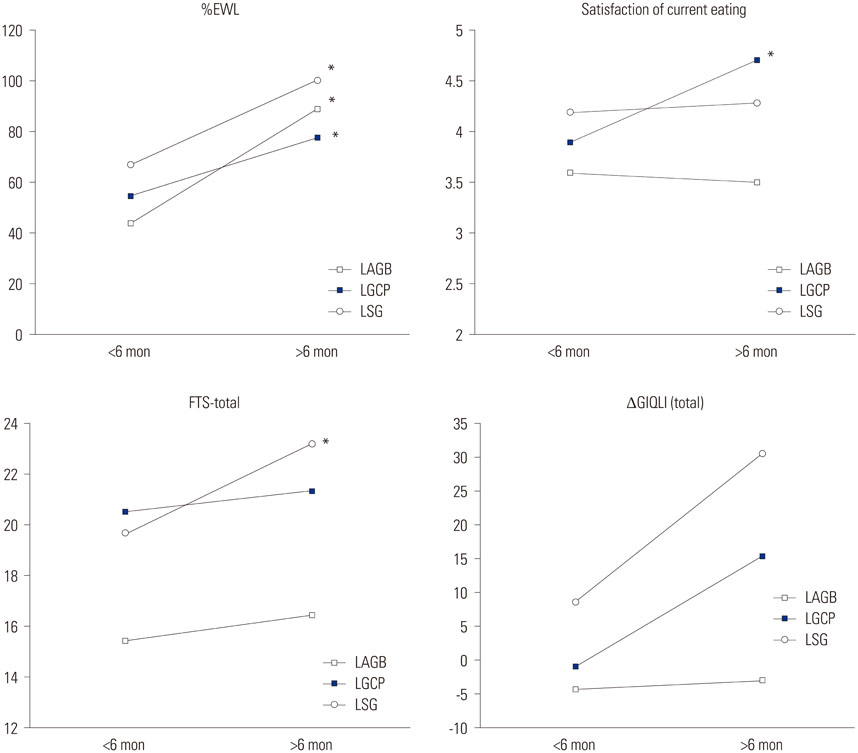
A total of 85 patients (LAGB=45, LGCP=22, and LSG=18) returned the questionnaires in full, and these patients constituted the study cohort. The cohort was predominately female (n=73, 85.9%). Mean percentage excess weight loss (%EWL) values after LAGB, LGCP, and LSG were 65.4+/-27.0%, 65.6+/-25.2%, and 82.7+/-21.7%, respectively (p=0.044). Mean postoperative FTSs and improvements in total GIQLIs after LAGB, LGCP, and LSG were 15.96, 20.95, and 21.33 and -3.40, 6.68, and 18.78, respectively (p<0.05). All procedures produced improvements in the three SF-36 domain scores. Subgroup analysis revealed significant differences between the three procedures in terms of improvements in general health and emotional well-being.
CONCLUSION
LGCP is safe and effective at achieving significant weight loss. In terms of food tolerance and GI quality of life, LGCP was found to be comparable to gastric banding and sleeve gastrectomy.
MeSH Terms
Figure
Cited by 1 articles
-
Short-Term Outcomes of Laparoscopic Greater Curvature Plication and Laparoscopic Sleeve Gastrectomy in Patients with a Body Mass Index of 30 to 35 kg/m2
Yeon Ho Park, Seong Min Kim
Yonsei Med J. 2017;58(5):1025-1030. doi: 10.3349/ymj.2017.58.5.1025.
Reference
-
1. Clinical Issues Committee. ASMBS policy statement on gastric plication. Surg Obes Relat Dis. 2011; 7:262.2. Ramos A, Galvao Neto M, Galvao M, Evangelista LF, Campos JM, Ferraz A. Laparoscopic greater curvature plication: initial results of an alternative restrictive bariatric procedure. Obes Surg. 2010; 20:913–918.
Article3. Brethauer SA, Harris JL, Kroh M, Schauer PR. Laparoscopic gastric plication for treatment of severe obesity. Surg Obes Relat Dis. 2011; 7:15–22.
Article4. Talebpour M, Amoli BS. Laparoscopic total gastric vertical plication in morbid obesity. J Laparoendosc Adv Surg Tech A. 2007; 17:793–798.
Article5. Niazi M, Maleki AR, Talebpour M. Short-term outcomes of laparoscopic gastric plication in morbidly obese patients: importance of postoperative follow-up. Obes Surg. 2013; 23:87–92.
Article6. Skrekas G, Antiochos K, Stafyla VK. Laparoscopic gastric greater curvature plication: results and complications in a series of 135 patients. Obes Surg. 2011; 21:1657–1663.
Article7. Mui WL, Lee DW, Lam KK, Tsung BY. Laparoscopic greater curve plication in Asia: initial experience. Obes Surg. 2013; 23:179–183.
Article8. Pujol Gebelli J, García Ruiz de Gordejuela A, Casajoana Badía A, Secanella Medayo L, Vicens Morton A, Masdevall Noguera C. [Laparoscopic Gastric Plication: a new surgery for the treatment of morbid obesity]. Cir Esp. 2011; 89:356–361.
Article9. Talebpour M, Motamedi SM, Talebpour A, Vahidi H. Twelve year experience of laparoscopic gastric plication in morbid obesity: development of the technique and patient outcomes. Ann Surg Innov Res. 2012; 6:7.
Article10. Suter M, Calmes JM, Paroz A, Giusti V. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007; 17:2–8.
Article11. Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmülling C, Neugebauer E, et al. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg. 1995; 82:216–222.
Article12. Robert M, Denis A, Badol-Van Straaten P, Jaisson-Hot I, Gouillat C. Prospective longitudinal assessment of change in health-related quality of life after adjustable gastric banding. Obes Surg. 2013; 23:1564–1570.
Article13. Bueter M, Maroske J, Thalheimer A, Gasser M, Stingl T, Heimbucher J, et al. Short- and long-term results of laparoscopic gastric banding for morbid obesity. Langenbecks Arch Surg. 2008; 393:199–205.
Article14. Champault A, Duwat O, Polliand C, Rizk N, Champault GG. Quality of life after laparoscopic gastric banding: prospective study (152 cases) with a follow-up of 2 years. Surg Laparosc Endosc Percutan Tech. 2006; 16:131–136.15. Dixon JB, O'Brien PE. Changes in comorbidities and improvements in quality of life after LAP-BAND placement. Am J Surg. 2002; 184(6B):51S–54S.
Article16. Caiazzo R, Arnalsteen L, Pigeyre M, Dezfoulian G, Verkindt H, Kirkby-Bott J, et al. Long-term metabolic outcome and quality of life after laparoscopic adjustable gastric banding in obese patients with type 2 diabetes mellitus or impaired fasting glucose. Br J Surg. 2010; 97:884–891.
Article17. Helmiö M, Salminen P, Sintonen H, Ovaska J, Victorzon M. A 5-year prospective quality of life analysis following laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2011; 21:1585–1591.
Article18. Pilone V, Mozzi E, Schettino AM, Furbetta F, Di Maro A, Giardiello C, et al. Improvement in health-related quality of life in first year after laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2012; 8:260–268.
Article19. Weiner R, Blanco-Engert R, Weiner S, Matkowitz R, Schaefer L, Pomhoff I. Outcome after laparoscopic adjustable gastric banding - 8 years experience. Obes Surg. 2003; 13:427–434.
Article20. Schweiger C, Weiss R, Keidar A. Effect of different bariatric operations on food tolerance and quality of eating. Obes Surg. 2010; 20:1393–1399.
Article21. Lee YC, Liew PL, Lee WJ, Lin YC, Lee CK. Gastrointestinal quality of life following bariatric surgery in Asian patients. Hepatogastroenterology. 2013; 60:759–761.22. Lee WK, Kim SM. Three-year experience of pouch dilatation and slippage management after laparoscopic adjustable gastric banding. Yonsei Med J. 2014; 55:149–156.
Article23. Yoon CI, Pak KH, Kim SM. Early experience with diagnosis and management of eroded gastric bands. J Korean Surg Soc. 2012; 82:18–27.
Article24. Park YH, Kim SM. Laparoscopic sleeve gastrectomy as revisional surgery for adjustable gastric band erosion. J Laparoendosc Adv Surg Tech A. 2014; 24:593–600.
Article25. Overs SE, Freeman RA, Zarshenas N, Walton KL, Jorgensen JO. Food tolerance and gastrointestinal quality of life following three bariatric procedures: adjustable gastric banding, Roux-en-Y gastric bypass, and sleeve gastrectomy. Obes Surg. 2012; 22:536–543.
Article26. Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013; 23:427–436.
Article27. Alley JB, Fenton SJ, Harnisch MC, Tapper DN, Pfluke JM, Peterson RM. Quality of life after sleeve gastrectomy and adjustable gastric banding. Surg Obes Relat Dis. 2012; 8:31–40.
Article28. Brunault P, Jacobi D, Léger J, Bourbao-Tournois C, Huten N, Camus V, et al. Observations regarding 'quality of life' and 'comfort with food' after bariatric surgery: comparison between laparoscopic adjustable gastric banding and sleeve gastrectomy. Obes Surg. 2011; 21:1225–1231.
Article29. D'Hondt M, Vanneste S, Pottel H, Devriendt D, Van Rooy F, Vansteenkiste F. Laparoscopic sleeve gastrectomy as a single-stage procedure for the treatment of morbid obesity and the resulting quality of life, resolution of comorbidities, food tolerance, and 6-year weight loss. Surg Endosc. 2011; 25:2498–2504.30. Watkins BM. Gastric compartment syndrome: an unusual complication of gastric plication surgery. Surg Obes Relat Dis. 2012; 8:e80–e81.
Article31. Tsang A, Jain V. Pitfalls of bariatric tourism: a complication of gastric plication. Surg Obes Relat Dis. 2012; 8:e77–e79.
Article32. El-Geidie A, Gad-el-Hak N. Laparoscopic gastric plication: technical report. Surg Obes Relat Dis. 2014; 10:151–154.
Article33. Lee WJ, Wang W, Yu PJ, Wei PL, Huang MT. Gastrointestinal quality of life following laparoscopic adjustable gastric banding in Asia. Obes Surg. 2006; 16:586–591.
Article34. Hussain A, Khan A, El-Hasani S. Laparoscopic management of ischemic gastric perforation after banded plication for obesity. Surg Obes Relat Dis. 2014; 10:745–746.
Article35. Atlas H, Yazbek T, Garneau PY, Safa N, Denis R. Is there a future for Laparoscopic Gastric Greater Curvature Plication (LGGCP)? A review of 44 patients. Obes Surg. 2013; 23:1397–1403.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-term Experience of Laparoscopic Greater Curvature Plication in Morbidly Obese Korean Patients
- Short-Term Outcomes of Laparoscopic Greater Curvature Plication and Laparoscopic Sleeve Gastrectomy in Patients with a Body Mass Index of 30 to 35 kg/m²
- Current Status of Laparoscopic Colectomy for Colon Cancer
- Long-term Functional and Patientreported Outcomes Between Intra-corporeal Delta-shaped Gastroduodenostomy and Gastrojejunostomy After Laparoscopic Distal Gastrectomy
- Effects of a Short-term Home-based Pulmonary Rehabilitation Program in Patients with Chronic Lung Disease