J Korean Med Sci.
2016 May;31(5):814-816. 10.3346/jkms.2016.31.5.814.
Calculation of the Residual Blood Volume after Acute, Non-Ongoing Hemorrhage Using Serial Hematocrit Measurements and the Volume of Isotonic Fluid Infused: Theoretical Hypothesis Generating Study
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea.
- 2Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea. 1tim4ezra7@gmail.com
- KMID: 2373683
- DOI: http://doi.org/10.3346/jkms.2016.31.5.814
Abstract
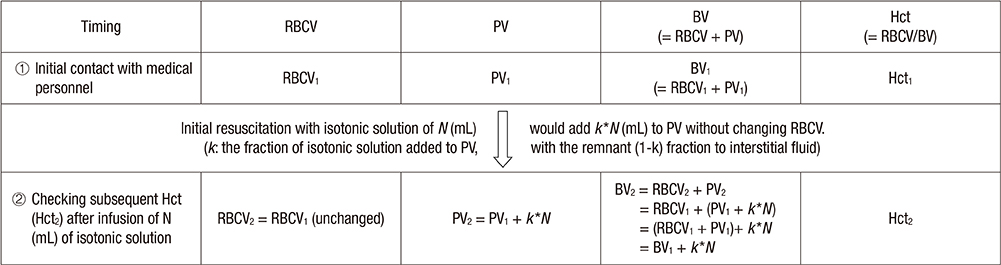
- Fluid resuscitation, hemostasis, and transfusion is essential in care of hemorrhagic shock. Although estimation of the residual blood volume is crucial, the standard measuring methods are impractical or unsafe. Vital signs, central venous or pulmonary artery pressures are inaccurate. We hypothesized that the residual blood volume for acute, non-ongoing hemorrhage was calculable using serial hematocrit measurements and the volume of isotonic solution infused. Blood volume is the sum of volumes of red blood cells and plasma. For acute, non-ongoing hemorrhage, red blood cell volume would not change. A certain portion of the isotonic fluid would increase plasma volume. Mathematically, we suggest that the residual blood volume after acute, non-ongoing hemorrhage might be calculated as 0·25N/[(Hct1/Hct2)-1], where Hct1 and Hct2 are the initial and subsequent hematocrits, respectively, and N is the volume of isotonic solution infused. In vivo validation and modification is needed before clinical application of this model.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A simple and novel equation to estimate the degree of bleeding in haemorrhagic shock: mathematical derivation and preliminary
in vivo validation
Sung-Bin Chon, Min Ji Lee, Won Sup Oh, Ye Jin Park, Joon-Myoung Kwon, Kyuseok Kim
Korean J Physiol Pharmacol. 2022;26(3):195-205. doi: 10.4196/kjpp.2022.26.3.195.
Reference
-
1. Norton R, Kobusingye O. Injuries. N Engl J Med. 2013; 368:1723–1730.2. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2095–2128.3. Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, Pons PT. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995; 38:185–193.4. Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, Browder T, Noguchi TT, Demetriades D. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007; 63:1338–1346.5. Rose AH, Kotzé A, Doolan D, Norfolk DR, Bellamy MC. Massive transfusion--evaluation of current clinical practice and outcome in two large teaching hospital trusts in Northern England. Vox Sang. 2009; 97:247–253.6. Spinella PC, Holcomb JB. Resuscitation and transfusion principles for traumatic hemorrhagic shock. Blood Rev. 2009; 23:231–240.7. American College of Surgeons, Committee on Trauma. ATLS, Advanced Trauma Life Support for Doctors: Student Course Manual. 8th ed. Chicago, IL: American College of Surgeons;2008.8. Kim Y, Lee K, Kim J, Kim J, Heo Y, Wang H, Lee K, Jung K. Application of damage control resuscitation strategies to patients with severe traumatic hemorrhage: review of plasma to packed red blood cell ratios at a single institution. J Korean Med Sci. 2014; 29:1007–1011.9. Valeri CR, Dennis RC, Ragno G, Macgregor H, Menzoian JO, Khuri SF. Limitations of the hematocrit level to assess the need for red blood cell transfusion in hypovolemic anemic patients. Transfusion. 2006; 46:365–371.10. Takanishi DM, Yu M, Lurie F, Biuk-Aghai E, Yamauchi H, Ho HC, Chapital AD. Peripheral blood hematocrit in critically ill surgical patients: an imprecise surrogate of true red blood cell volume. Anesth Analg. 2008; 106:1808–1812.11. Oohashi S, Endoh H. Does central venous pressure or pulmonary capillary wedge pressure reflect the status of circulating blood volume in patients after extended transthoracic esophagectomy? J Anesth. 2005; 19:21–25.12. Shippy CR, Appel PL, Shoemaker WC. Reliability of clinical monitoring to assess blood volume in critically ill patients. Crit Care Med. 1984; 12:107–112.13. Iijima T, Iwao Y, Sankawa H. Circulating blood volume measured by pulse dye-densitometry: comparison with (131)I-HSA analysis. Anesthesiology. 1998; 89:1329–1335.14. Jones JG, Wardrop CA. Measurement of blood volume in surgical and intensive care practice. Br J Anaesth. 2000; 84:226–235.15. Marik PE, Monnet X, Teboul JL. Hemodynamic parameters to guide fluid therapy. Ann Intensive Care. 2011; 1:1.16. Drobin D, Hahn RG. Volume kinetics of Ringer’s solution in hypovolemic volunteers. Anesthesiology. 1999; 90:81–91.17. Imm A, Carlson RW. Fluid resuscitation in circulatory shock. Crit Care Clin. 1993; 9:313–333.18. Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev. 2013; 2:CD000567.19. Ryan ML, Thorson CM, Otero CA, Vu T, Schulman CI, Livingstone AS, Proctor KG. Initial hematocrit in trauma: a paradigm shift? J Trauma Acute Care Surg. 2012; 72:54–59.20. Norberg A, Brauer KI, Prough DS, Gabrielsson J, Hahn RG, Uchida T, Traber DL, Svensén CH. Volume turnover kinetics of fluid shifts after hemorrhage, fluid infusion, and the combination of hemorrhage and fluid infusion in sheep. Anesthesiology. 2005; 102:985–994.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A simple and novel equation to estimate the degree of bleeding in haemorrhagic shock: mathematical derivation and preliminary in vivo validation
- Effect of Hypertonic Fluid Resuscitation in Major Burn Injury
- Autotransfusion in Intracranial Aneurysmal Surgery Perioperative Blood Collection and Acute Hemodilution
- Effects of anesthesia on fluid volume kinetics after infusion of colloid solution during blood donation
- The Predictors of the Change of Cardiac Output and the Changes of Electrolyte in the Acute Hemorrhagic Dogs