Korean J Gastroenterol.
2015 Aug;66(2):111-115. 10.4166/kjg.2015.66.2.111.
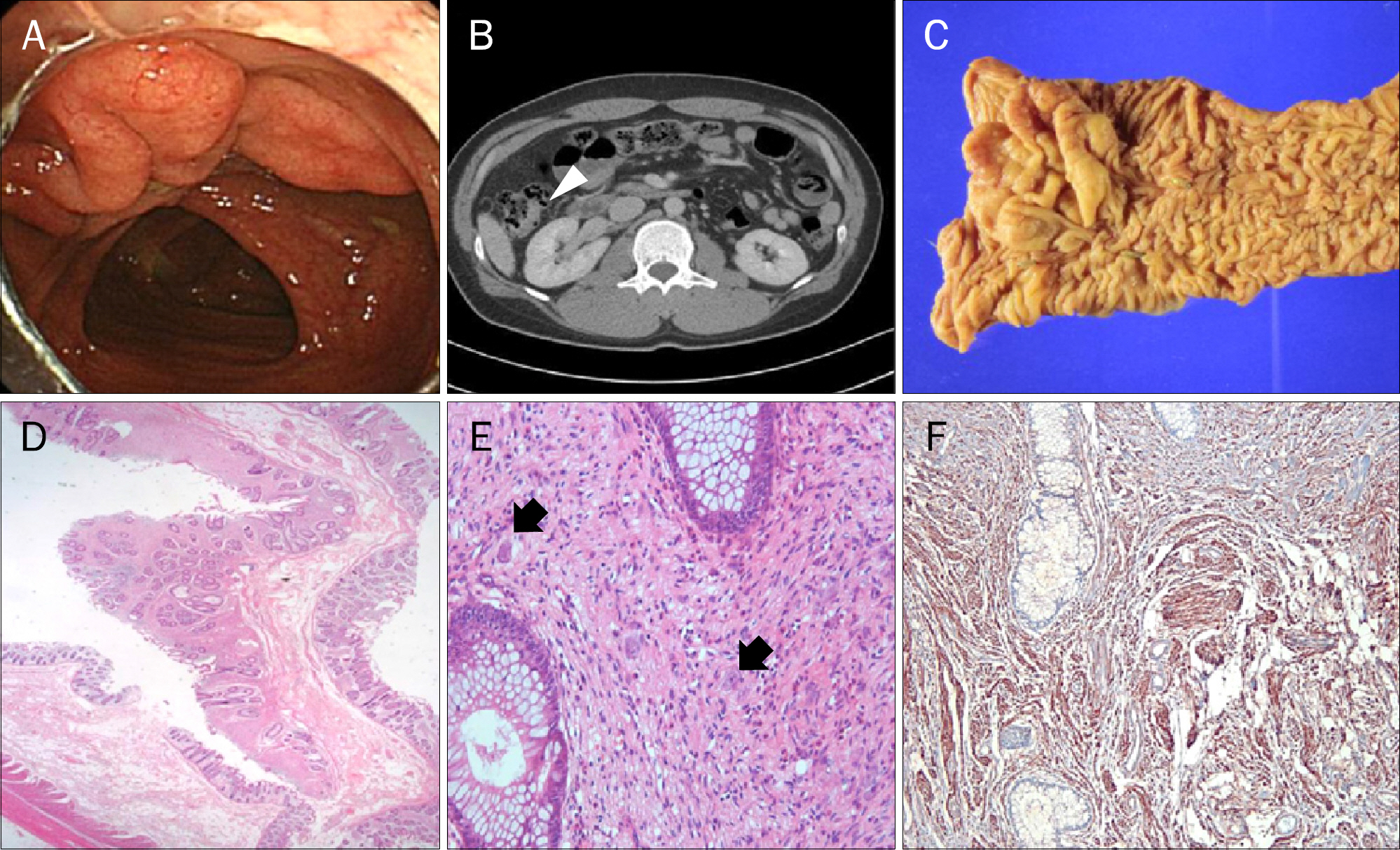
Diffuse Ganglioneuromatosis of the Colon Presenting as a Large Subepithelial Tumor in Adults: Report of Two Cases
- Affiliations
-
- 1Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea. hlim77@hallym.or.kr
- 2Department of Pathology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- 3Department of Surgery, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- KMID: 2373323
- DOI: http://doi.org/10.4166/kjg.2015.66.2.111
Abstract
- Colonic diffuse ganglioneuromatosis is a benign neoplastic condition characterized by disseminated, intramural, or transmural proliferation of neural elements involving the enteric plexuses, sometimes associated with von Recklinghausen's disease and other multiple tumor syndromes. Colonic diffuse ganglioneuromatosis is usually large, ranging from 1 to 17 cm, and thus can distort the surrounding tissue architecture as well as infiltrate the adjacent bowel wall. However, colonic diffuse ganglioneuromatosis is an exceptional finding in adults and only individual cases are reported in the literature. Herein, we report two unusual cases of adult patients with colonic diffuse transmural ganglioneuromatosis presenting as a large subepithelial tumor.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Shekitka KM, Sobin LH. Ganglioneuromas of the gastrointestinal tract. Relation to Von Recklinghausen disease and other multiple tumor syndromes. Am J Surg Pathol. 1994; 18:250–257.2. Chambonnière ML, Porcheron J, Scoazec JY, Audigier JC, Mosnier JF. Intestinal ganglioneuromatosis diagnosed in adult patients. Gastroenterol Clin Biol. 2003; 27:219–224.3. Mateş I, Iosif C, Dinu D, Constantinoiu S. Solitary ganglioneuromatosis of the descending colon, presenting as giant retroperitoneal tumour. Chirurgia (Bucur). 2013; 108:584–588.4. Jung YW, Jang BI, Chang KA, Kim KO, Kim MJ. The solitary polypoid ganglioneuroma of the ascending colon. Korean J Gastrointest Endosc. 2010; 41:390–393.5. Bang BW, Jeong S, Kim CH, et al. A case of polypoid ganglioneuroma of the colon. Korean J Gastrointest Endosc. 2008; 36:48–51.6. Kim SH, Choi CH, Paik YH, Kim WH, Kim H. Isolated polypoid ganglioneuroma in the rectum. Korean J Pathol. 2001; 35:344–346.7. Park JY, Kang YN, Park KS, Choe M. Solitary polypoid ganglioneuroma of the cecum. J Korean Soc Coloproctol. 2009; 25:264–267.
Article8. Miettinen M, Fletcher CDM, Kindblom LG, Tsui WMS. Mesechimal tumors of the colon and rectum. Bosman FT, Carneiro F, Hruman RH, Theise ND, editors. WHO classification of tumours of the digestive system. 4th ed.Lion: IARC;2010. p. 140–141.9. DeSchryver-Kecskemeti K, Clouse RE, Goldstein MN, Gersell D, O'Neal L. Intestinal ganglioneuromatosis. A manifestation of overproduction of nerve growth factor? N Engl J Med. 1983; 308:635–639.10. Srinivasan R, Mayle JE. Polypoid ganglioneuroma of colon. Dig Dis Sci. 1998; 43:908–909.11. Carney JA, Go VL, Sizemore GW, Hayles AB. Alimentary-tract ganglioneuromatosis. A major component of the syndrome of multiple endocrine neoplasia, type 2b. N Engl J Med. 1976; 295:1287–1291.12. Hochberg FH, Dasilva AB, Galdabini J, Richardson EP Jr. Gastrointestinal involvement in von Recklinghausen's neurofibromatosis. Neurology. 1974; 24:1144–1151.
Article13. DiLiberti JH, Weleber RG, Budden S. Ruvalcaba-Myhre-Smith syndrome: a case with probable autosomal-dominant inheritance and additional manifestations. Am J Med Genet. 1983; 15:491–495.
Article14. Urschel JD, Berendt RC, Anselmo JE. Surgical treatment of colonic ganglioneuromatosis in neurofibromatosis. Can J Surg. 1991; 34:271–276.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of colon cancer in a patient with longstanding colonic diffuse ganglioneuromatosis: a case report
- Diffuse Ganglioneuromatosis of Appendix associated with Von Recklinghausen;s Disease
- Polypoid Ganglioneuromatosis of Colon: A case report
- A Case of Ganglioneuromatosis of the Colon
- Intestinal Ganglioneuromatosis in a Pediatric Patient Presenting as Perforation: A Case Report and Literature Review