Korean J Gastroenterol.
2015 Jul;66(1):41-45. 10.4166/kjg.2015.66.1.41.
A Case of Intra-abdominal Paragonimiasis Mimicking Metastasis of Lung Cancer Diagnosed by Endoscopic Ultrasound-guided Fine Needle Aspiration
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. lkhyuck@gmail.com
- KMID: 2373310
- DOI: http://doi.org/10.4166/kjg.2015.66.1.41
Abstract
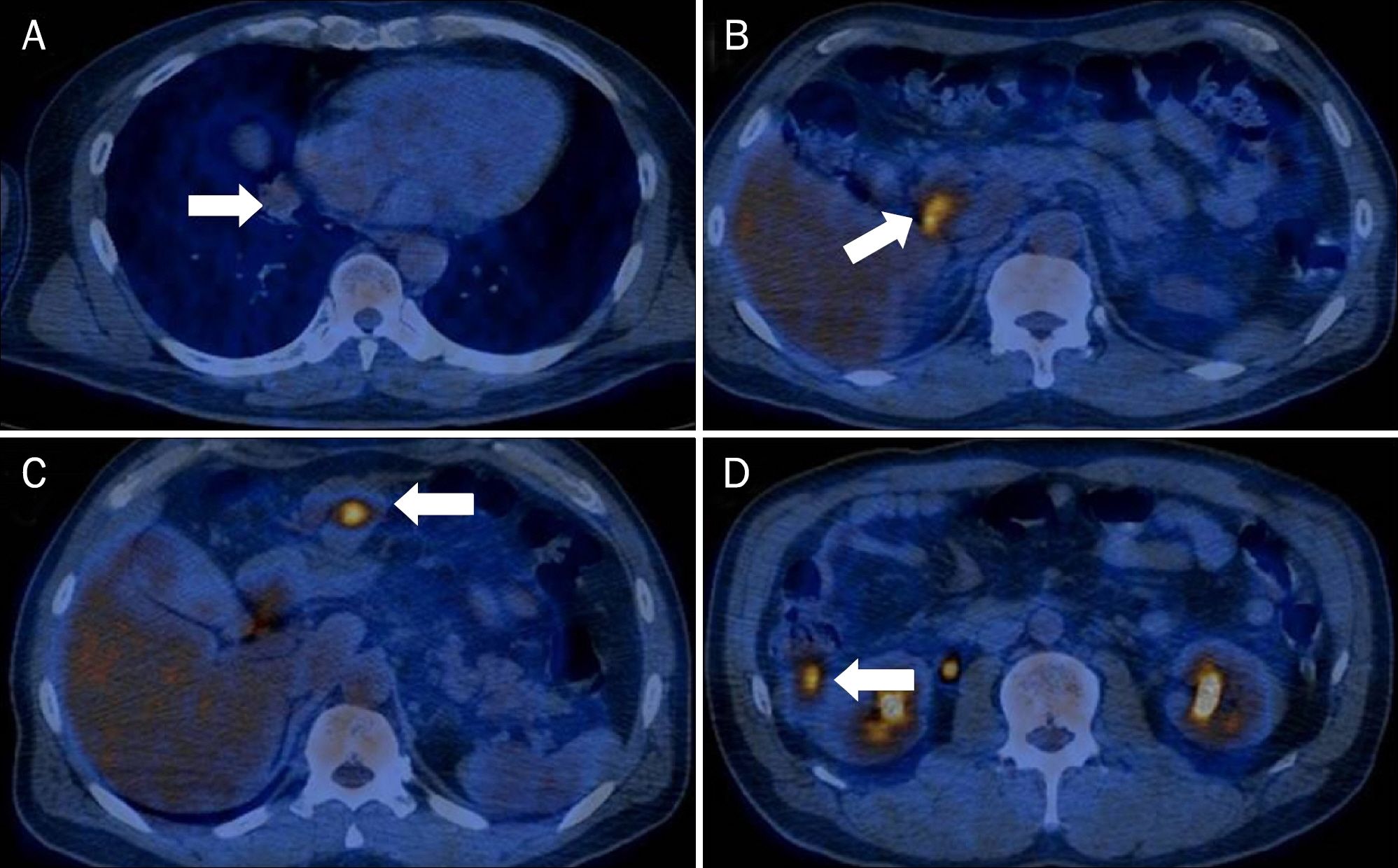
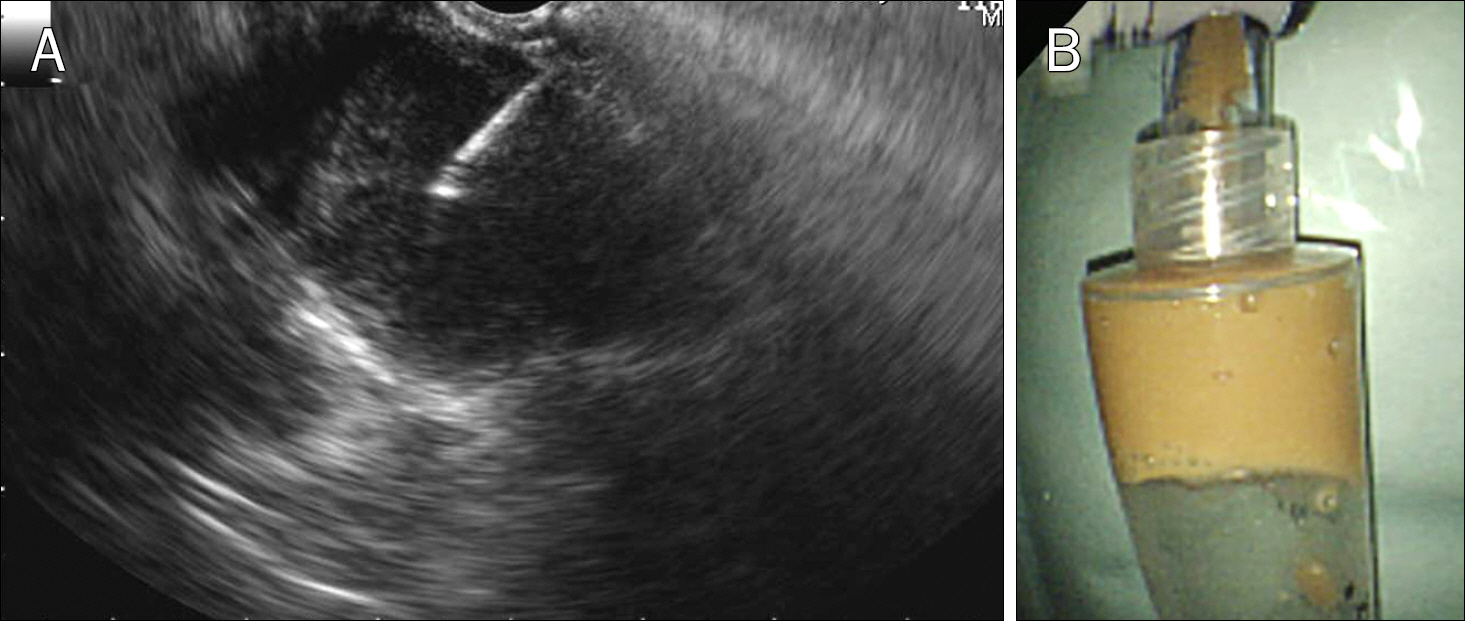
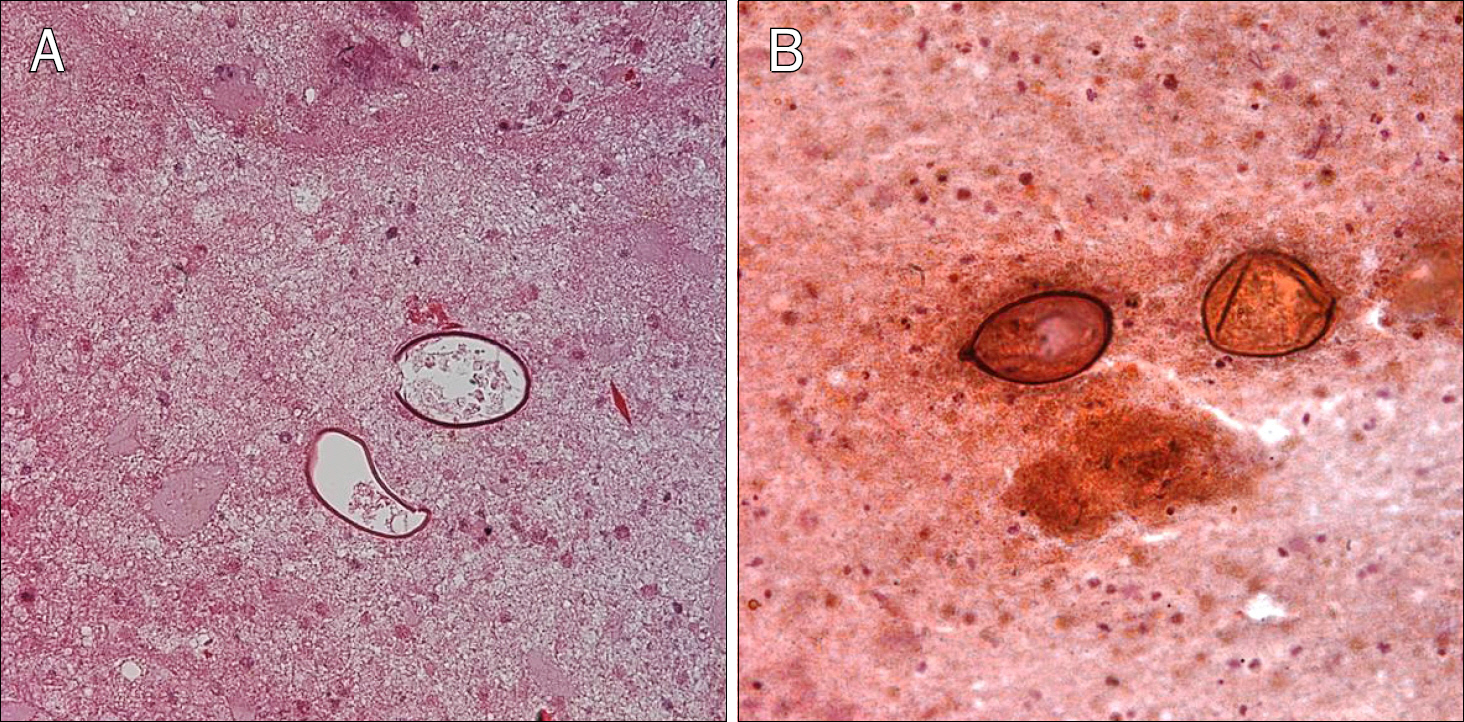
- Paragonimiasis has been continuously decreasing in Korea. However, it still occurs by ingesting raw or incompletely cooked fresh water crab or crayfish. The diagnosis of paragonimiasis is challenging because of its rarity. It may be confused with other inflammatory disease or carcinomatosis. Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) has lower risk of complications such as bleeding, perforation than percutaneous fine needle aspiration. EUS-FNA is more accurate and popular method to find mucosal or submucosal tumors and the lesions of several organs. Benign and malignant tumors, infectious diseases have been diagnosed by EUS-FNA, but there was no report describing the use of EUS-FNA for diagnosing paragonimiasis. Herein, we present a 47-year-old male patient with paragonimiasis diagnosed by EUS-FNA. Imaging studies revealed mass lesions in the lung and peritoneal cavity, which was eventually confirmed as paragonimiasis using EUS-FNA.
MeSH Terms
Figure
Cited by 2 articles
-
A Paragonimiasis Mimicking Gastric Submucosal Tumor
Hyeri Seok, Tae Sung Sohn, Kyong Ran Peck
J Korean Med Sci. 2019;34(6):. doi: 10.3346/jkms.2019.34.e45.Status of common parasitic diseases in Korea in 2019
Sun Huh
J Korean Med Assoc. 2019;62(8):437-456. doi: 10.5124/jkma.2019.62.8.437.
Reference
-
References
1. Lee CH, Kim JH, Moon WS, Lee MR. Paragonimiasis in the abdominal cavity and subcutaneous tissue: report of 3 cases. Korean J Parasitol. 2012; 50:345–347.
Article2. Choi DW. Paragonimus and paragonimiasis in Korea. Kisaengchunghak Chapchi. 1990; 28(Suppl):79–102.
Article3. Catalano MF, Sial S, Chak A, et al. EUS-guided fine needle aspiration of idiopathic abdominal masses. Gastrointest Endosc. 2002; 55:854–858.
Article4. Costache MI, Iordache S, Karstensen JG, Săftoiu A, Vilmann P. Endoscopic ultrasound-guided fine needle aspiration: from the past to the future. Endosc Ultrasound. 2013; 2:77–85.
Article5. Jeon K, Koh WJ, Kim H, et al. Clinical features of recently diagnosed pulmonary paragonimiasis in Korea. Chest. 2005; 128:1423–1430.
Article6. Kim AY. Heterotopic paragonimiasis presented by intraabdominal masses. Korean J Gastroenterol. 2013; 61:351–353.
Article7. Kim TS, Han J, Shim SS, et al. Pleuropulmonary paragonimiasis: CT findings in 31 patients. AJR Am J Roentgenol. 2005; 185:616–621.
Article8. Kim KU, Lee K, Park HK, Jeong YJ, Yu HS, Lee MK. A pulmonary paragonimiasis case mimicking metastatic pulmonary tumor. Korean J Parasitol. 2011; 49:69–72.
Article9. Lee JJ, Choi CM, Kwon HH, et al. A case of pulmonary paragonimiasis mimicking lung cancer diagnosed by EBUS-TBNA. Korean J Med. 2013; 84:423–427.
Article10. Kim EY. Linear array endoscopic ultrasonography 1. Korean J Gastrointest Endosc. 2009; 38:1–8.11. Eloubeidi MA, Tamhane A. Prospective assessment of diagnostic utility and complications of endoscopic ultrasound-guided fine needle aspiration. Results from a newly developed academic endoscopic ultrasound program. Dig Dis. 2008; 26:356–363.12. Jenssen C, Dietrich CF. Endoscopic ultrasound-guided finenee-dle aspiration biopsy and trucut biopsy in gastroenterology – An overview. Best Pract Res Clin Gastroenterol. 2009; 23:743–759.
Article13. O'Toole D, Palazzo L, Arotçarena R, et al. Assessment of complications of EUS-guided fine-needle aspiration. Gastrointest Endosc. 2001; 53:470–474.14. Carter JE, Nelson JJ, Eves M, Boudreaux C. Giardia lamblia infection diagnosed by endoscopic ultrasound-guided fine-nee-dle aspiration. Diagn Cytopathol. 2007; 35:363–365.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How Can We Get the Best Results with Endoscopic Ultrasound-Guided Fine Needle Aspiration?
- Role of endoscopic ultrasound in non-small cell lung cancer
- A Case of Pulmonary Paragonimiasis Mimicking Lung Cancer Diagnosed by EBUS-TBNA
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?
- The Role of EBUS-TBNA in the Diagnosis and Staging of Lung Cancer