J Dent Rehabil Appl Sci.
2016 Dec;32(4):301-306. 10.14368/jdras.2016.32.4.301.
Overdenture with magnetic attachments for a patient with Parkinson's disease: a case report
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Chonnam National University, Gwangju, Republic of Korea. mcnihil@jnu.ac.kr
- KMID: 2369070
- DOI: http://doi.org/10.14368/jdras.2016.32.4.301
Abstract
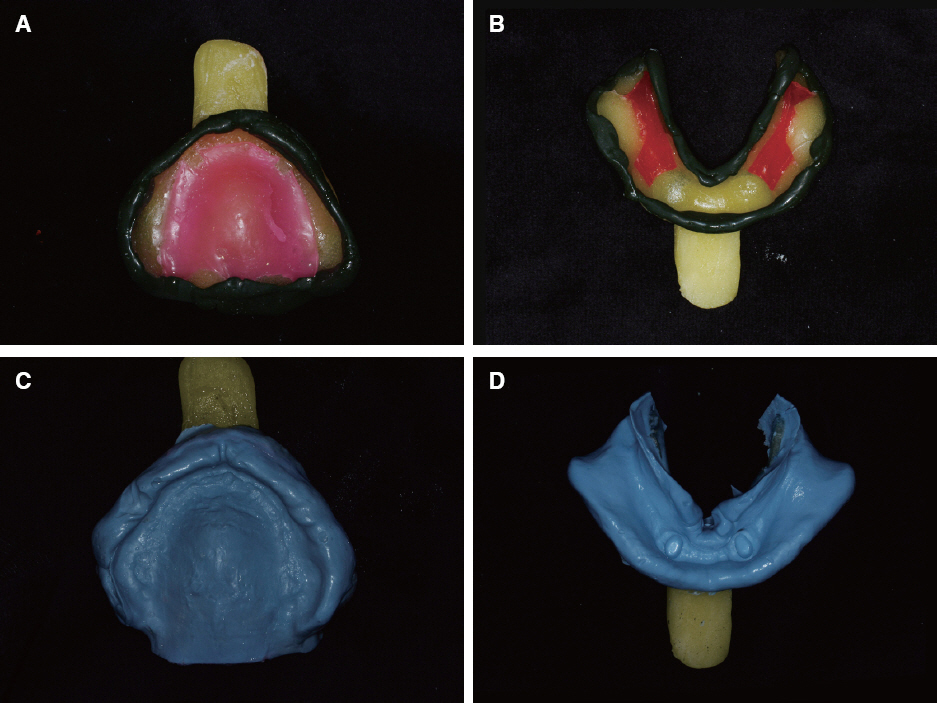
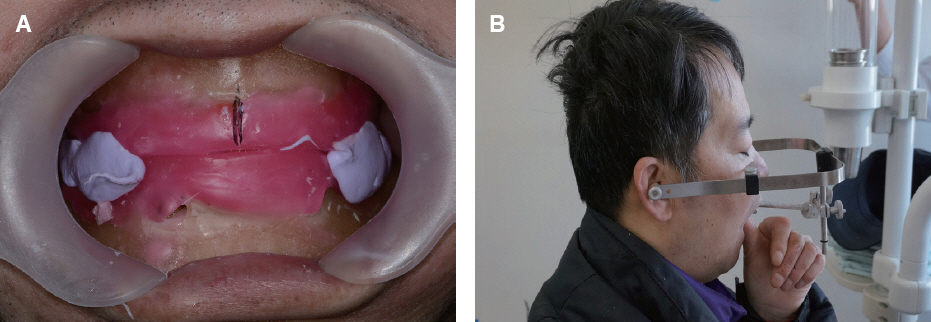
- It is very hard for edentulous patients to satisfy retention and stability with their complete denture. Especially, for patients with systemic diseases such as Parkinson's disease causing involuntary and limited movements, fabricating complete dentures may be challenging to both dentists and patients due to functional limitations. To overcome this problem, overdentures can be used through conserving retained roots. In this case, a 45-year-old male patient had to extract numerous teeth due to dental caries, and at the time of visit he was taking drugs for diabetes and Parkinson's disease for a period of long time. A complete denture was applied to maxilla, and for mandible, an overdenture on two preserved retained roots was applied where its retention and stability were obtained by magnetic attachments. This case reports that overdenture with retained roots improved overall functional limitations.
MeSH Terms
Figure
Reference
-
References
1. Kim SU. Implant-supported removable prosthetic treatments with patient focus. Myungmoon: Seoul;2007.2. Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969; 3:81–100. DOI: 10.3109/02844316909036699. PMID: 4924041.3. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981; 10:387–416. DOI: 10.1016/S0300-9785(81)80077-4.4. Riley MA, Walmsley AD, Harris IR. Magnets in prosthetic dentistry. J Prosthet Dent. 2001; 86:13742. DOI: 10.1067/mpr.2001.115533. PMID: 11514799.5. Smith GA, Laird WR, Grant AA. Magnetic retention units for overdentures. J Oral Rehabil. 1983; 10:481–8. DOI: 10.1111/j.1365-2842.1983.tb01471.x. PMID: 6358436.6. Packer M, Nikitin V, Coward T, Davis DM, Fiske J. The potential benefits of dental implants on the oral health quality of life of people with Parkinson’s disease. Gerodontology. 2009; 26:11–8. DOI: 10.1111/j.1741-2358.2008.00233.x. PMID: 19278520.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overdentures of the patient with Parkinson's disease: A case report
- The Implant Retained Overdenture by Locator Attachments on the Edentulous Mandible: A Case Report
- A study on the changes in attractive force of magnetic attachments for overdenture
- Maxillary implant-supported overdenture with magnetic attachment using healing abutment: A case report
- Implant-supported milled bar overdenture with two implant surgical guides