J Korean Orthop Assoc.
2016 Dec;51(6):473-478. 10.4055/jkoa.2016.51.6.473.
Change in Neural Tube Size for a Lumbar Spinal Stenosis Patient on Axial Loading Magnetic Resonance Imaging
- Affiliations
-
- 1Department of Orthopaedic Surgery, Wonkwang University Sanbon Hospital, Gunpo, Korea.
- 2Department of Orthopaedic Surgery, Wonkwang University School of Medicine, Iksan, Korea. osktg@wonkwang.ac.kr
- KMID: 2364298
- DOI: http://doi.org/10.4055/jkoa.2016.51.6.473
Abstract
- PURPOSE
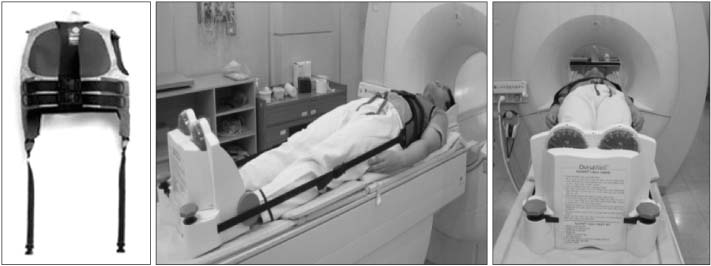
A conventional magnetic resonance imaging (MRI) was conducted in supine position, showing a slight different from that conducted in upright position. Therefore, we simulated the upright position by applying the axial load on a lumbar spinal stenosis patient and measured the change of neural tube size in axial load and standardized the data.
MATERIALS AND METHODS
We compared the axial loading MRI obtained from spinal stenosis patients who visited Wonkwang University Hospital outpatient clinic between October 2010 and May 2011 showing radiologic and physical symptoms.
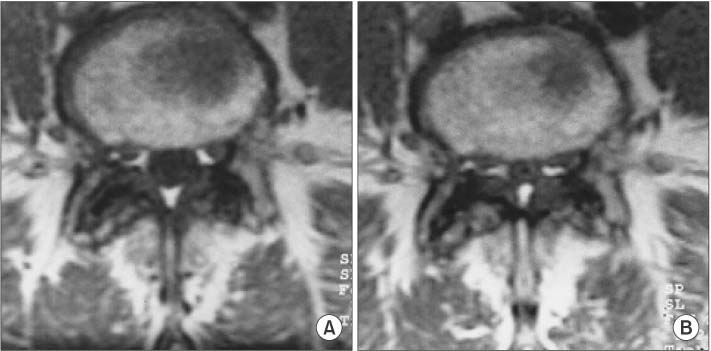
RESULTS
Neural tube sizes by conventional MRI were as follows: 195.57 mm² and 203.20 mm² on average between the left and right sides in L3/4; 194.64 mm² and 211.43 mm² on average in L4/5; and 199.38 mm² and 203.04 mm² on average in L5/S1. Neural tube sizes by axial loading MRI were as follows: 166.43 mm² and 174.27 mm² on average between the left and right sides in L3/4; 154.81 mm² and 158.67 mm² on average in L4/5; and 148.48 mm² and 157.19 mm² on average in L5/S1. Changes of neural tube sizes in L3/4, L4/5, and L5/S1 had a significant correlation (p<0.05).
CONCLUSION
The axial loading device was an excellent tool in simulating the upright position for spinal stenosis patients, and the change of neural tube sizes reproduced for the upright position was statistically significant. This is thought to be meaningful for clinical applicability.
MeSH Terms
Figure
Reference
-
1. Rho YW, Song JE, Byun CS, Shin KS. Spinal stenosis. J Korean Orthop Assoc. 1985; 20:1037–1044.
Article2. Jinkins JR, Dworkin JS, Damadian RV. Upright, weight-bearing, dynamic-kinetic MRI of the spine: initial results. Eur Radiol. 2005; 15:1815–1825.
Article3. Huang KY, Lin RM, Lee YL, Li JD. Factors affecting disability and physical function in degenerative lumbar spondylolisthesis of L4-5: evaluation with axially loaded MRI. Eur Spine J. 2009; 18:1851–1857.
Article4. Haughton VM. MR imaging of the spine. Radiology. 1988; 166:297–301.
Article5. Masaryk TJ, Ross JS, Modic MT, Boumphrey F, Bohlman H, Wilber G. High-resolution MR imaging of sequestered lumbar intervertebral disks. AJR Am J Roentgenol. 1988; 150:1155–1162.
Article6. Modic MT, Pavlicek W, Weinstein MA, et al. Magnetic resonance imaging of intervertebral disk disease. Clinical and pulse sequence considerations. Radiology. 1984; 152:103–111.
Article7. Epstein JA, Epstein BS, Lavin L. Nerve rot compression associated with narrowing of the lumbar spinal canal. J Neurol Neurosurg Psychiatry. 1962; 25:165–176.8. Winston K, Rumbaugh C, Colucci V. The vertebral canals in lumbar disc disease. Spine (Phila Pa 1976). 1984; 9:414–417.
Article9. Dora C, Wälchli B, Elfering A, Gal I, Weishaupt D, Boos N. The significance of spinal canal dimensions in discriminating symptomatic from asymptomatic disc herniations. Eur Spine J. 2002; 11:575–581.
Article10. Elsberg CA, Dyke CG. Diagnosis and localization of tumors of spinal cord by means of measurements made on X-ray films of vertebrae and the correlation of clinical and X-ray findings. Bull Neurol Inst NY. 1934; 3:359–375.11. Verbiest H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 1954; 36:230–237.
Article12. Gill GG, White H. Mechanisms of nerve-root compression and irritation in backache; surgical decompression in intervertebral disk conditions; spondylolisthesis, spina bifida occulta and transitional fifth lumbar vertebra. Clin Orthop. 1955; 5:66–81.13. Porter RW, Wicks M, Ottewell D. Measurement of the spinal canal by diagnostic ultrasound. J Bone Joint Surg Br. 1978; 60:481–484.
Article14. Kimura S, Steinbach GC, Watenpaugh DE, Hargens AR. Lumbar spine disc height and curvature responses to an axial load generated by a compression device compatible with magnetic resonance imaging. Spine (Phila Pa 1976). 2001; 26:2596–2600.
Article15. Lee SU, Hargens AR, Fredericson M, Lang PK. Lumbar spine disc heights and curvature: upright posture vs. supine compression harness. Aviat Space Environ Med. 2003; 74:512–516.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Morphological Analysis of the Cervical Spinal Cord, Dural Tube, and Spinal Canal by Magnetic Resonance Imaging in Normal Korean Adults
- Magnetic Resonance Imaging Grading Systems for Central Canal and Neural Foraminal Stenoses of the Lumbar and Cervical Spines With a Focus on the Lee Grading System
- Effect of Axial loading on Lumbar spine MRI: Comparative Study of Effect between a Patient Group with Claudication and a Patient Group without Claudication
- Dynamic Lumbar Spinal Stenosis : The Usefulness of Axial Loaded MRI in Preoperative Evaluation
- Congenital Absence of a Pedicle of L4 in the Spinal Stenosis: A Case Report