Clin Orthop Surg.
2016 Mar;8(1):119-122. 10.4055/cios.2016.8.1.119.
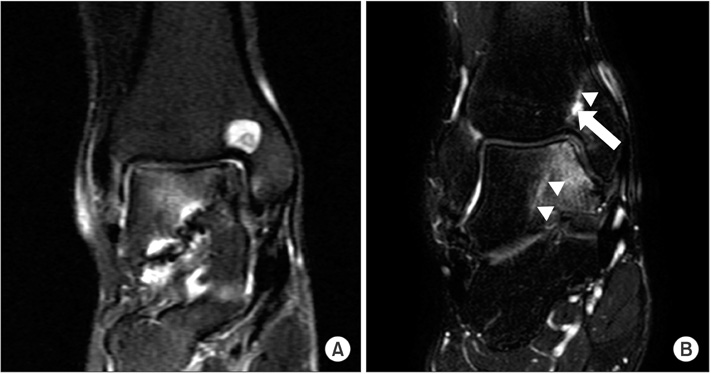
Is Antegrade Transmalleolar Drilling Method for Osteochondral Lesion of Talus Necessary? Iatrogenic Cystic Formation at the Tibia: A Report of Five Cases
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea. leewoochun@gmail.com
- 2Department of Orthopaedic Surgery, Asian Hospital and Medical Center, Muntinlupa, Philippines.
- KMID: 2363956
- DOI: http://doi.org/10.4055/cios.2016.8.1.119
Abstract
- Antegrade transmalleolar drilling method is one of the options for the treatment of osteochondral lesion of talus (OLT). We present five patients who underwent tibial drilling for treatment of OLT and later developed distal tibial cystic formation induced by cartilage opening or heat necrosis during drilling. Antegrade transmalleolar drilling can be a possible option for the treatment of OLT if the lesion is not easily reachable; however, other viable treatment should be considered due to its possibility of distal tibial pathologic change.
Keyword
MeSH Terms
Figure
Reference
-
1. Simonian PT, Wickiewicz TL, O'Brien SJ, Dines JS, Schatz JA, Warren RF. Pretibial cyst formation after anterior cruciate ligament surgery with soft tissue autografts. Arthroscopy. 1998; 14(2):215–220.
Article2. Olech E, Sicher H, Weinmann JP. Traumatic mandibular bone cysts. Oral Surg Oral Med Oral Pathol. 1951; 4(9):1160–1172.
Article3. Crane AR, Scarano JJ. Synovial cysts (ganglia) of bone: report of two cases. J Bone Joint Surg Am. 1967; 49(2):355–361.4. Kumai T, Takakura Y, Higashiyama I, Tamai S. Arthroscopic drilling for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1999; 81(9):1229–1235.
Article5. Rhinelander FW. Tibial blood supply in relation to fracture healing. Clin Orthop Relat Res. 1974; (105):34–81.
Article6. Berman AT, Reid JS, Yanicko DR Jr, Sih GC, Zimmerman MR. Thermally induced bone necrosis in rabbits: relation to implant failure in humans. Clin Orthop Relat Res. 1984; (186):284–292.7. Lundskog J. Heat and bone tissue: an experimental investigation of the thermal properties of bone and threshold levels for thermal injury. Scand J Plast Reconstr Surg. 1972; 9:1–80.8. Bonfield W, Li CH. The temperature dependence of the deformation of bone. J Biomech. 1968; 1(4):323–329.
Article9. Eriksson AR, Albrektsson T. Temperature threshold levels for heat-induced bone tissue injury: a vital-microscopic study in the rabbit. J Prosthet Dent. 1983; 50(1):101–107.
Article10. D'Hooghe P, Deschamps K, Matricali G. Iatrogenic osteochondral kissing lesion after transmalleolar drilling of the talar dome: a case report. J Am Podiatr Med Assoc. 2009; 99(1):54–57.11. Bechtol CO, Ferguson AB Jr, Laing PG. Metals and engineering in bone and joint surgery. Baltimore: Williams & Wilkins;1959.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Results of the Multiple Drilling for Osteochondral Lesion of the Medial Talar Dome
- Autologous Osteochondral Transplantation as a Secondary Procedure after Failed Microfracture for Osteochondral Lesion of Talus
- Osteochondral Lesion of the Tibial Plafond: A Case Report
- Simultaneously Occurred Medial and Lateral Osteochondral Lesions of the Talus
- Redomicrofracture as a Treatment for Osteochondral Lesion of Talus after the Failure of Arthroscopic Microfracture