Korean J Ophthalmol.
2015 Dec;29(6):368-374. 10.3341/kjo.2015.29.6.368.
Surgical Outcomes of Canalicular Trephination Combined with Endoscopic Dacryocystorhinostomy in Patients with Distal or Common Canalicular Obstruction
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. ysyat01@naver.com
- 2Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea.
- KMID: 2363843
- DOI: http://doi.org/10.3341/kjo.2015.29.6.368
Abstract
- PURPOSE
This study investigated the surgical outcomes of canalicular trephination combined with endoscopic dacryocystorhinostomy (DCR) in patients with a distal or common canalicular obstruction. It also identified the factors affecting surgical success rates associated with this technique.
METHODS
We retrospectively reviewed the medical records of 57 patients (59 eyes) in whom a canalicular obstruction was encountered during endoscopic DCR. All patients were treated with endoscopic DCR, followed by canalicular trephination and silicone tube placement. The surgical outcome was categorized as a functional success according to the patient's subjective assessment of symptoms, including epiphora, and as an anatomical success according to a postoperative nasolacrimal duct irrigation test. Surgical success rates were compared based on age, sex, location of the obstruction, number of silicone tubes, and experience of the surgeon.
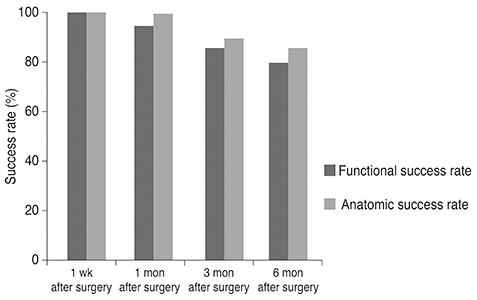
RESULTS
Functional success was achieved in 55 of 59 eyes (93%) at one month, 50 eyes (84%) at three months, and 46 eyes (78%) at six months. Anatomical success was achieved in 58 of 59 eyes (98%) at one month, 52 eyes (88%) at three months, and 50 eyes (84%) at six months. There was a statistically significant difference in surgical outcome according to the experience of the surgeon. The anatomical success rate at the six-month follow-up exam was 95.4% in the >5 years of experience group, and 53.3% in the <5 years of experience group (p = 0.008, Pearson chi-square test).
CONCLUSIONS
The success rate of canalicular trephination combined with endoscopic DCR in patients with a distal or common canalicular obstruction decreased gradually during the six-month follow-up period. In particular, patients undergoing procedures with experienced surgeons tended to show excellent surgical outcomes at the six-month follow-up exam.
MeSH Terms
Figure
Cited by 2 articles
-
Efficacy of Intraoperative Mitomycin C Eye Drops during and after Dacryocystorhinostomy for Canalicular Obstruction
Yu-Jin Choi, Seong Jae Kim, Ji Myong Yoo, Seong Wook Seo
J Korean Ophthalmol Soc. 2018;59(10):899-907. doi: 10.3341/jkos.2018.59.10.899.Management of Nasolacrimal Duct Obstruction: ENT Surgeon’s Perspective
Young-Jun Chung
Korean J Otorhinolaryngol-Head Neck Surg. 2017;60(10):481-490. doi: 10.3342/kjorl-hns.2017.00745.
Reference
-
1. Nemet AY, Wilcsek G, Francis IC. Endoscopic dacryocystorhinostomy with adjunctive mitomycin C for canalicular obstruction. Orbit. 2007; 26:97–100.2. Welham RA, Henderson PH. Results of dacryocystorhinostomy analysis of causes for failure. Trans Ophthalmol Soc U K. 1973; 93:601–609.3. Boboridis K, Ziakas N, Georgiadis N. Nasolacrimal intubation with mitomycin C. Ophthalmology. 2004; 111:416–417.4. Baek BJ, Hwang GR, Jung DH, et al. Surgical results of endoscopic dacryocystorhinostomy and lacrimal trephination in distal or common canalicular obstruction. Clin Exp Otorhinolaryngol. 2012; 5:101–106.5. Boboridis KG, Bunce C, Rose GE. Outcome of external dacryocystorhinostomy combined with membranectomy of a distal canalicular obstruction. Am J Ophthalmol. 2005; 139:1051–1055.6. Narioka J, Ohashi Y. Transcanalicular-endonasal semiconductor diode laser-assisted revision surgery for failed external dacryocystorhinostomy. Am J Ophthalmol. 2008; 146:60–68.7. Hwang SW, Khwarg SI, Kim JH, et al. Bicanalicular double silicone intubation in external dacryocystorhinostomy and canaliculoplasty for distal canalicular obstruction. Acta Ophthalmologica. 2009; 87:438–442.8. Khoubian JF, Kikkawa DO, Gonnering RS. Trephination and silicone stent intubation for the treatment of canalicular obstruction: effect of the level of obstruction. Ophthal Plast Reconstr Surg. 2006; 22:248–252.9. Jones LT. The cure of epiphora due to canalicular disorders, trauma and surgical failures on the lacrimal passages. Trans Am Acad Ophthalmol Otolaryngol. 1962; 66:506–524.10. Jones LT. Conjunctivodacryocystorhinostomy. Am J Ophthalmol. 1965; 59:773–783.11. Nathoo NA, Rath S, Wan D, Buffam F. Trephination for canalicular obstruction: experience in 45 eyes. Orbit. 2013; 32:281–284.12. You YG, Choi HS, Ryou JH, Kim SJ. The results of endoscopic canaliculocystodacryorhinostomy with two sets of silicone tube intubation in canalicular obstruction. J Korean Ophthalmol Soc. 2004; 45:882–886.13. Kim SJ, Kim SD. The surgical results of endonasal DCR with two silicone tubes in common canalicular obstruction. J Korean Ophthalmol Soc. 2007; 48:1170–1176.14. Paik JS, Cho WK, Yang SW. Bicanalicular double silicone stenting in endoscopic dacryocystorhinostomy with lacrimal trephination in distal or common canalicular obstruction. Eur Arch Otorhinolaryngol. 2012; 269:1605–1611.15. Chong KK, Lai FH, Ho M, et al. Randomized trial on silicone intubation in endoscopic mechanical dacryocystorhinostomy (SEND) for primary nasolacrimal duct obstruction. Ophthalmology. 2013; 120:2139–2145.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
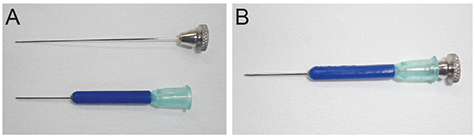
- Canalicular Trephination with Lacrimal Trephine and Endoscopic DCR
- Surgical Results of Endoscopic Dacryocystorhinostomy and Lacrimal Trephination in Distal or Common Canalicular Obstruction
- Surgical Results of Lacrimal Surgery with or without Canalicular Stenosis
- Canaliculodacryocystorhinostomy in Canalicular Obstruction
- The Surgical Results of Endonasal DCR with Two Silicone Tubes in Common Canalicular Obstruction