J Periodontal Implant Sci.
2016 Dec;46(6):415-425. 10.5051/jpis.2016.46.6.415.
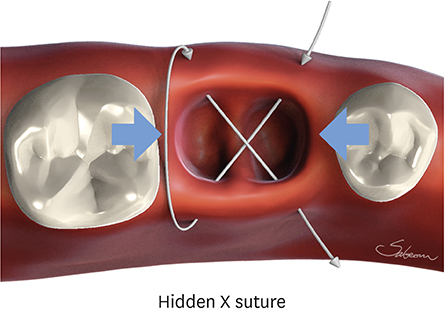
The hidden X suture: a technical note on a novel suture technique for alveolar ridge preservation
- Affiliations
-
- 1Department of Periodontology, Dankook University College of Dentistry, Cheonan, Korea. periopark@dankook.ac.kr
- 2Department of Periodontology, Seoul National University School of Dentistry, Seoul, Korea.
- 3Department of Periodontology, Kyung Hee University School of Dentistry, Seoul, Korea.
- KMID: 2362907
- DOI: http://doi.org/10.5051/jpis.2016.46.6.415
Abstract
- PURPOSE
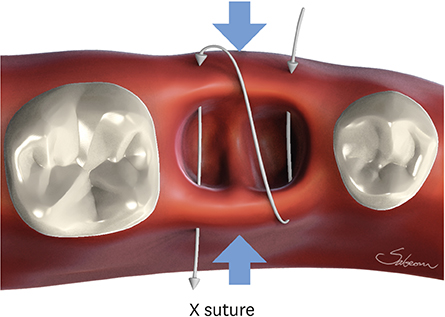
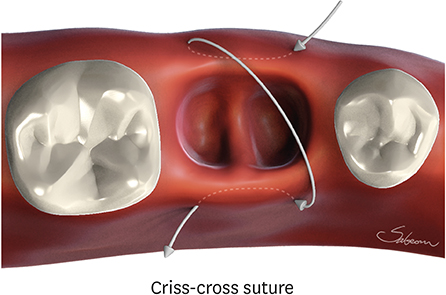
The present study investigated the impact of 2 different suture techniques, the conventional crossed mattress suture (X suture) and the novel hidden X suture, for alveolar ridge preservation (ARP) with an open healing approach.
METHODS
This study was a prospective randomized controlled clinical trial. Fourteen patients requiring extraction of the maxillary or mandibular posterior teeth were enrolled and allocated into 2 groups. After extraction, demineralized bovine bone matrix mixed with 10% collagen (DBBM-C) was grafted and the socket was covered by porcine collagen membrane in a double-layer fashion. No attempt to obtain primary closure was made. The hidden X suture and conventional X suture techniques were performed in the test and control groups, respectively. Cone-beam computed tomographic (CBCT) images were taken immediately after the graft procedure and before implant surgery 4 months later. Additionally, the change in the mucogingival junction (MGJ) position was measured and was compared after extraction, after suturing, and 4 months after the operation.
RESULTS
All sites healed without any complications. Clinical evaluations showed that the MGJ line shifted to the lingual side immediately after the application of the X suture by 1.56±0.90 mm in the control group, while the application of the hidden X suture rather pushed the MGJ line slightly to the buccal side by 0.25±0.66 mm. It was demonstrated that the amount of keratinized tissue (KT) preserved on the buccal side was significantly greater in the hidden X suture group 4 months after the procedure (P<0.05). Radiographic analysis showed that the hidden X suture had a significant effect in preserving horizontal width and minimizing vertical reduction in comparison to X suture (P<0.05).
CONCLUSIONS
Our study provided clinical and radiographic verification of the efficacy of the hidden X suture in preserving the width of KT and the dimensions of the alveolar ridge after ARP.
MeSH Terms
Figure
Cited by 2 articles
-
Alveolar ridge preservation with an open-healing approach using single-layer or double-layer coverage with collagen membranes
Ho-Keun Choi, Hag-Yeon Cho, Sung-Jo Lee, In-Woo Cho, Hyun-Seung Shin, Ki-Tae Koo, Hyun-Chang Lim, Jung-Chul Park
J Periodontal Implant Sci. 2017;47(6):372-380. doi: 10.5051/jpis.2017.47.6.372.A comparison of different compressive forces on graft materials during alveolar ridge preservation
In-Woo Cho, Jung-Chul Park, Hyun-Seung Shin
J Periodontal Implant Sci. 2017;47(1):51-63. doi: 10.5051/jpis.2017.47.1.51.
Reference
-
1. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003; 23:313–323.2. Wang RE, Lang NP. Ridge preservation after tooth extraction. Clin Oral Implants Res. 2012; 23:Suppl 6. 147–156.
Article3. Araújo MG, Liljenberg B, Lindhe J. Dynamics of Bio-Oss Collagen incorporation in fresh extraction wounds: an experimental study in the dog. Clin Oral Implants Res. 2010; 21:55–64.
Article4. Araújo MG, Lindhe J. Ridge preservation with the use of Bio-Oss collagen: a 6-month study in the dog. Clin Oral Implants Res. 2009; 20:433–440.
Article5. Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler MB. Hard tissue alterations after socket preservation: an experimental study in the beagle dog. Clin Oral Implants Res. 2008; 19:1111–1118.
Article6. Jung RE, Philipp A, Annen BM, Signorelli L, Thoma DS, Hämmerle CH, et al. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clin Periodontol. 2013; 40:90–98.
Article7. Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009; 20:545–549.
Article8. Rothamel D, Schwarz F, Herten M, Chiriac G, Pakravan N, Sager M, et al. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. Mund Kiefer Gesichtschir. 2007; 11:89–97.9. Barone A, Ricci M, Tonelli P, Santini S, Covani U. Tissue changes of extraction sockets in humans: a comparison of spontaneous healing vs. ridge preservation with secondary soft tissue healing. Clin Oral Implants Res. 2013; 24:1231–1237.
Article10. Engler-Hamm D, Cheung WS, Yen A, Stark PC, Griffin T. Ridge preservation using a composite bone graft and a bioabsorbable membrane with and without primary wound closure: a comparative clinical trial. J Periodontol. 2011; 82:377–387.
Article11. Horváth A, Mardas N, Mezzomo LA, Needleman IG, Donos N. Alveolar ridge preservation. A systematic review. Clin Oral Investig. 2013; 17:341–363.
Article12. Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L, Cardaropoli G. Socket preservation using bovine bone mineral and collagen membrane: a randomized controlled clinical trial with histologic analysis. Int J Periodontics Restorative Dent. 2012; 32:421–430.13. Glocker M, Attin T, Schmidlin PR. Ridge preservation with modified “socket-shield” technique: a methodological case series. Dent J. 2014; 2:11–21.
Article14. Gomes OM, Amaral AS, Gonçalves AJ, Brito AS, Monteiro EL. New suture techniques for best esthetic skin healing. Acta Cir Bras. 2012; 27:505–508.
Article15. Kim SH, Kim DY, Kim KH, Ku Y, Rhyu IC, Lee YM. The efficacy of a double-layer collagen membrane technique for overlaying block grafts in a rabbit calvarium model. Clin Oral Implants Res. 2009; 20:1124–1132.
Article16. Kozlovsky A, Aboodi G, Moses O, Tal H, Artzi Z, Weinreb M, et al. Bio-degradation of a resorbable collagen membrane (Bio-Gide) applied in a double-layer technique in rats. Clin Oral Implants Res. 2009; 20:1116–1123.
Article17. Darby I, Chen ST, Buser D. Ridge preservation techniques for implant therapy. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 260–271.18. Ten Heggeler JM, Slot DE, Van der Weijden GA. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: a systematic review. Clin Oral Implants Res. 2011; 22:779–788.
Article19. Brito C, Tenenbaum HC, Wong BK, Schmitt C, Nogueira-Filho G. Is keratinized mucosa indispensable to maintain peri-implant health? A systematic review of the literature. J Biomed Mater Res B Appl Biomater. 2014; 102:643–650.
Article20. Gobbato L, Avila-Ortiz G, Sohrabi K, Wang CW, Karimbux N. The effect of keratinized mucosa width on peri-implant health: a systematic review. Int J Oral Maxillofac Implants. 2013; 28:1536–1545.
Article21. Lin GH, Chan HL, Wang HL. The significance of keratinized mucosa on implant health: a systematic review. J Periodontol. 2013; 84:1755–1767.
Article22. Souza AB, Tormena M, Matarazzo F, Araújo MG. The influence of peri-implant keratinized mucosa on brushing discomfort and peri-implant tissue health. Clin Oral Implants Res. 2016; 27:650–655.
Article23. Park JC, Yang KB, Choi Y, Kim YT, Jung UW, Kim CS, et al. A simple approach to preserve keratinized mucosa around implants using a pre-fabricated implant-retained stent: a report of two cases. J Periodontal Implant Sci. 2010; 40:194–200.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Secure and Convenient Three-point and Multi-point Suture Technique
- Subclavian Portal Approach for Isolated Subscapularis Tendon Tear: Technical Note
- Anteroinferior Capsulolabral Complex Repair Using Antegrade Suture Passer: Technical Note
- Suture technique for successful guided bone regeneration; Preliminary report of double layered suture technique with subgingival suture
- Improving oral rehabilitation through the preservation of the tissues through alveolar preservation