J Korean Ophthalmol Soc.
2016 Dec;57(12):1970-1975. 10.3341/jkos.2016.57.12.1970.
A Case of Acute Macular Neuroretinopathy after Non-ocular Trauma
- Affiliations
-
- 1Department of Ophthalmology, Catholic University of Daegu School of Medicine, Daegu, Korea. yykim@cu.ac.kr
- KMID: 2362718
- DOI: http://doi.org/10.3341/jkos.2016.57.12.1970
Abstract
- PURPOSE
In the present study, an unusual case of traumatic retinopathy presenting as acute macular neuroretinopathy was reported.
CASE SUMMARY
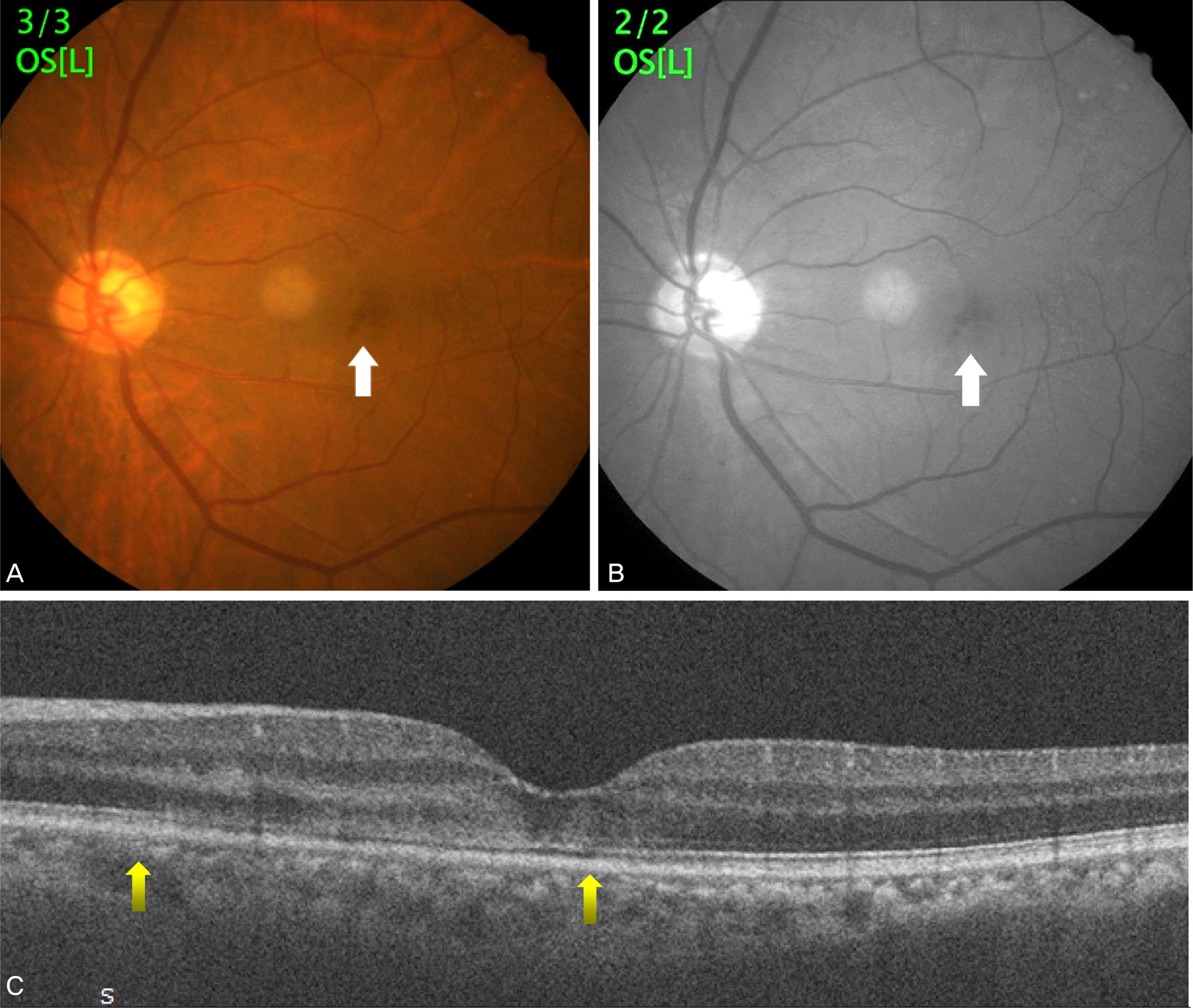
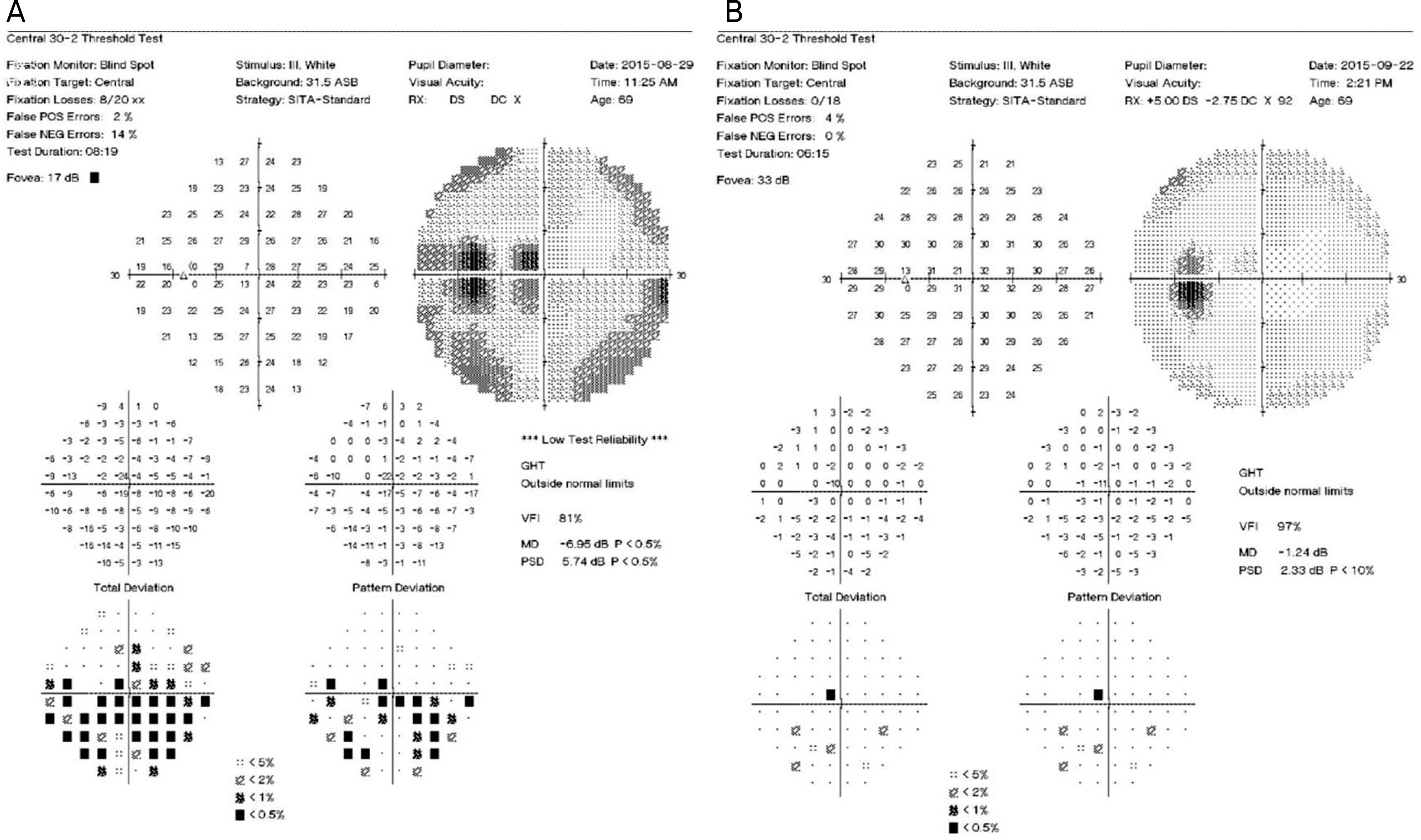
A 69-year-old male was involved in a car accident and experienced a left 5th rib fracture. There was no direct ocular trauma. However, after the accident he noticed paracentral scotoma and loss of vision in his left eye. At initial examination 4 days after the trauma, central visual acuity was hand motion and visual field test revealed central scotoma in the left eye. Spectral domain optical coherence tomography showed hyper-reflectivity of the outer nuclear layer and disruption of the ellipsoid zone. Fluorescein angiography did not show any leakage or vascular damage but near-infrared autofluorescence imaging showed a dark lesion in the macular area. Visual acuity was improved to 0.2 at 2 weeks after trauma and 0.6 at 6 months after trauma while mild ellipsoid zone defect and visual field defect persisted.
CONCLUSIONS
Traumatic retinopathy presenting as acute macular neuroretinopathy is an uncommon disease causing paracentral scotomas after non-ocular trauma, and to the best of our knowledge, this is the first reported case in Korea.
MeSH Terms
Figure
Reference
-
References
1. Bos PJ, Deutman AF. Acute macular neuroretinopathy. Am J Ophthalmol. 1975; 80:573–84.
Article2. Fawzi AA, Pappuru RR, Sarraf D, et al. Acute macular neuroretinopathy: long-term insights revealed by multimodal imaging. Retina. 2012; 32:1500–13.3. Bhavsar KV, Lin S, Rahimy E, et al. Acute macular neuroretinopathy: a comprehensive review of the literature. Surv Ophthalmol. 2016; 61:538–65.
Article4. Yu S, Wang F, Pang CE, et al. Multimodal imaging findings in abdominall deep capillary ischemia. Retina. 2014; 34:636–46.5. Sarraf D, Rahimy E, Fawzi AA, et al. Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy abdominal with retinal capillary ischemia. JAMA Ophthalmol. 2013; 131:1275–87.6. Rahimy E, Sarraf D. Paracentral acute middle maculopathy abdominal-domain optical coherence tomography feature of deep abdominal ischemia. Curr Opin Ophthalmol. 2014; 25:207–12.7. Chen X, Rahimy E, Sergott RC, et al. Spectrum of retinal vascular diseases associated with paracentral acute middle maculopathy. Am J Ophthalmol. 2015; 160:26–34.e1.
Article8. Gillies M, Sarks J, Dunlop C, Mitchell P. Traumatic retinopathy abdominal acute macular neuroretinopathy. Aust N Z J Ophthalmol. 1997; 25:207–10.9. Nentwich MM, Leys A, Cramer A, Ulbig MW. Traumatic abdominal presenting as acute macular neuroretinopathy. Br J abdominal. 2013; 97:1268–72.10. Chinskey ND, Rahimy E, Johnson MW. Acute macular abdominal following non-ocular trauma: a hypothesis regarding pathophysiologic mechanism. Ophthalmic Surg Lasers Imaging Retina. 2015; 46:1013–20.11. Feigl B, Haas A. Optical coherence tomography (OCT) in acute macular neuroretinopathy. Acta Ophthalmol Scand. 2000; 78:714–6.
Article12. Yeh S, Hwang TS, Weleber RG, et al. Acute macular outer abdominal (AMOR): a reappraisal of acute macular neuroretinopathy using multimodality diagnostic testing. Arch Ophthalmol. 2011; 129:365–8.13. Davies CL, Newman RJ, Molyneux SG, Grahame-Smith DG. The relationship between plasma catecholamines and severity of injury in man. J Trauma. 1984; 24:99–105.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Bilateral Acute Macular Neuroretinopathy after URI
- A Case of Acute Macular Neuroretinopathy in a Young Male
- Hyphema, angle recession and macular hemorrhage induced by air bag
- Spontaneous reattachment of retinal detachment with macular hole in nonmyopic patients
- Eccentric Macular Hole Formation After Macular Hole Surgery