Korean J Sports Med.
2016 Jun;34(1):36-42. 10.5763/kjsm.2016.34.1.36.
Biomechanical Parameters in Arch Building Gait Measured by Gait Analysis System with Pressure Sensor
- Affiliations
-
- 1Department of Rehabilitation and Physical Medicine, Kyung Hee University Hospital, Seoul, Korea.
- 2Department of Rehabilitation and Physical Medicine, Kyung Hee University Hospital at Gangdong, Seoul, Korea. tjg819@hanmail.net
- 3Department of Rehabilitation and Physical Medicine, Bethesda Hospital, Suwon, Korea.
- 4Korea Orthopedics and Rehabilitation Engineering Center, Incheon, Korea.
- KMID: 2361667
- DOI: http://doi.org/10.5763/kjsm.2016.34.1.36
Abstract
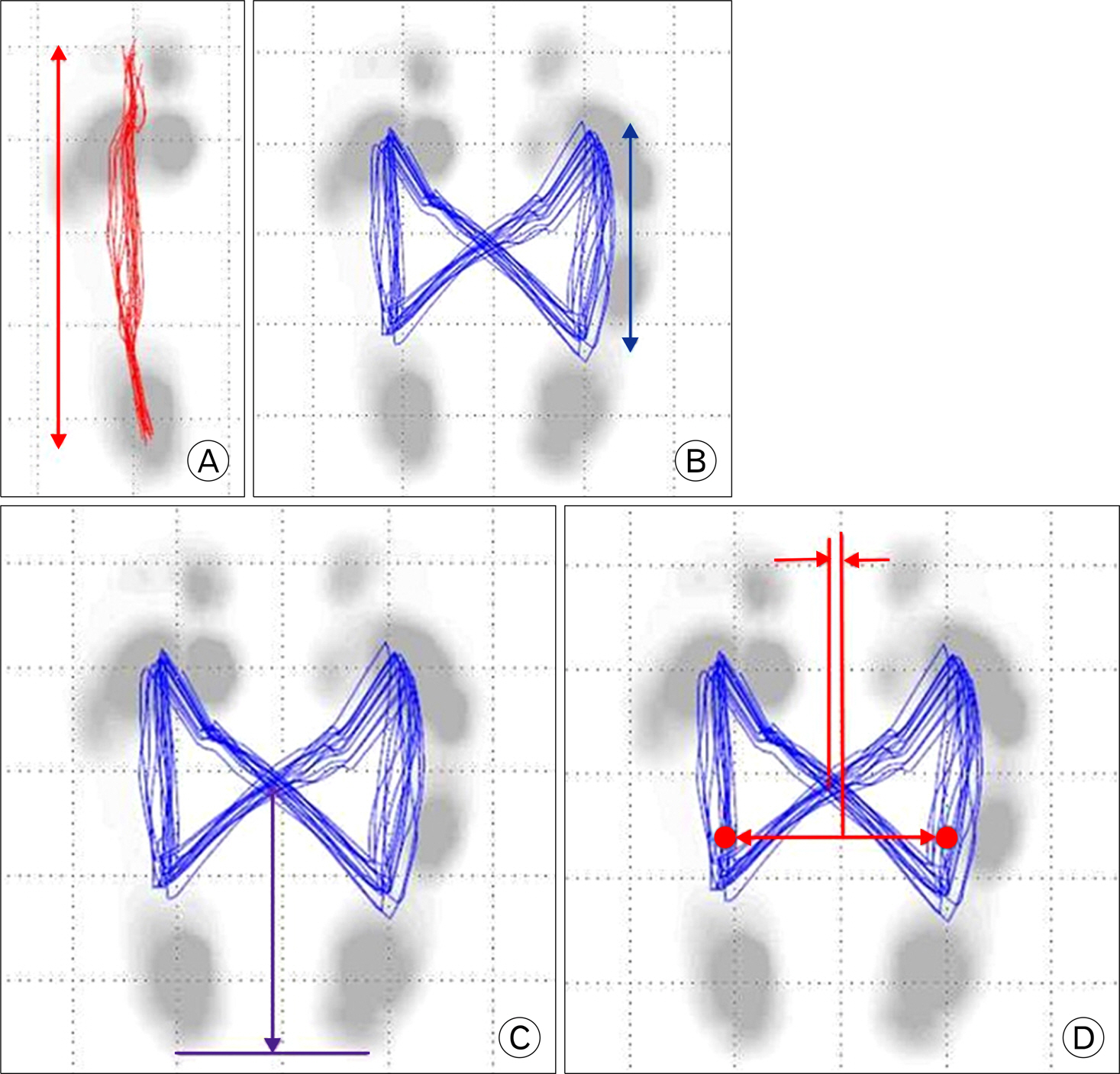
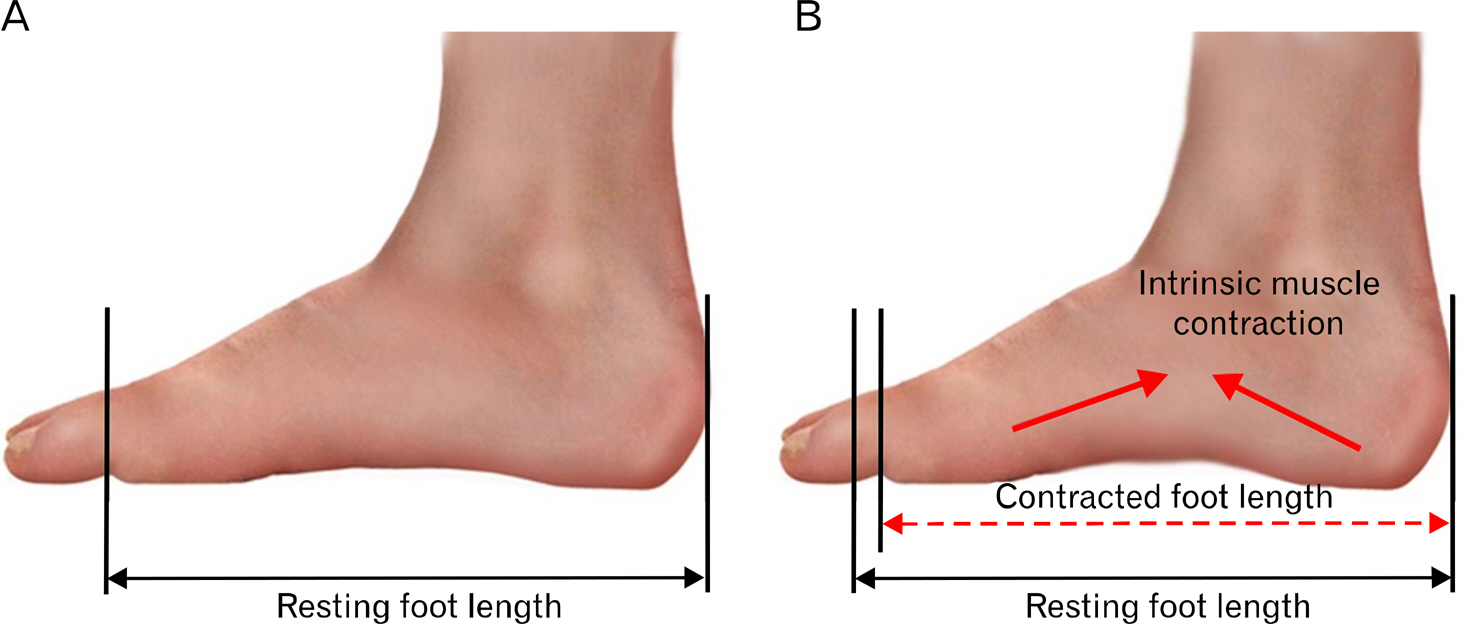
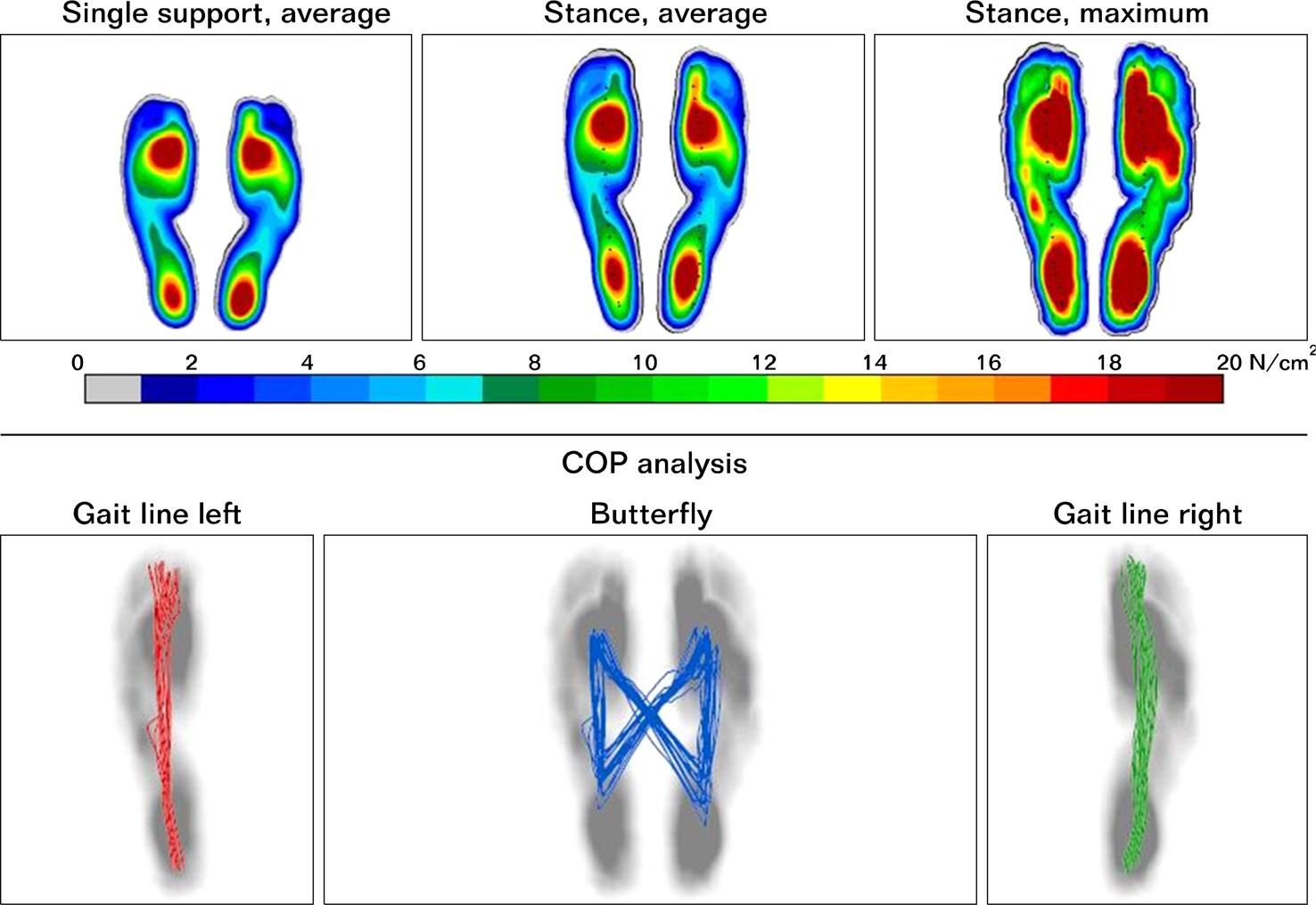
- The objective of study was to compare biomechanical parameters between normal and arch building gait in healthy subjects. A total of 40 feet from 20 healthy adults were evaluated in this study. The participants were asked to walk on a treadmill comfortably at 2 km/hr for 30 seconds. Then, they were asked to walk after making arch building through raising arches with their feet by pulling the big toe toward the heel. Gait parameters such as geometry, center of pressure, maximum force, and maximum pressure were measured in normal and the arch building gait using a gait analysis system equipped with pressure sensor. Arch building gait demonstrated significantly (p<0.01) decreased forefoot maximum force but significantly (p=0.024) increased heel maximum force compared to normal gait. Maximum pressures of the midfoot and heel were also significantly (both p<0.01) increased. However, the maximum pressures of the forefoot were not significantly (p>0.05) different between the two conditions. Geometry, phase, and time parameters were not significantly (p>0.05) different between the two conditions, either. Although forefoot and midfoot maximum force were significantly decreased in arch building gait compared to those in normal gait, the maximum pressure of forefoot was not significantly changed, indicating decreased area of forefoot contact during arch building gait. The arch building gait moves the center of presser to the hind foot and redistributes the contact area, thus changing the distribution of maximum pressure.
Keyword
Figure
Reference
-
1.Nurzynska D., Di Meglio F., Castaldo C, et al. Flatfoot in children: anatomy of decision making. Ital J Anat Embryol. 2012. 117:98–106.2.Ker RF., Bennett MB., Bibby SR., Kester RC., Alexander RM. The spring in the arch of the human foot. Nature. 1987. 325:147–9.
Article3.Ogon M., Aleksiev AR., Pope MH., Wimmer C., Saltzman CL. Does arch height affect impact loading at the lower back level in running? Foot Ankle Int. 1999. 20:263–6.
Article4.Huang CK., Kitaoka HB., An KN., Chao EY. Biomechanical evaluation of longitudinal arch stability. Foot Ankle. 1993. 14:353–7.
Article5.Mulligan EP., Cook PG. Effect of plantar intrinsic muscle training on medial longitudinal arch morphology and dynamic function. Man Ther. 2013. 18:425–30.
Article6.Jung DY., Koh EK., Kwon OY. Effect of foot orthoses and short-foot exercise on the cross-sectional area of the abductor hallucis muscle in subjects with pes planus: a randomized controlled trial. J Back Musculoskelet Rehabil. 2011. 24:225–31.7.Headlee DL., Leonard JL., Hart JM., Ingersoll CD., Hertel J. Fatigue of the plantar intrinsic foot muscles increases navicular drop. J Electromyogr Kinesiol. 2008. 18:420–5.
Article8.Mostert S., Kesselring J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult Scler. 2002. 8:161–8.9.Moon DC., Kim K., Lee SK. Immediate effect of short-foot exercise on dynamic balance of subjects with excessively pronated feet. J Phys Ther Sci. 2014. 26:117–9.10.Lynn SK., Padilla RA., Tsang KK. Differences in static- and dynamic-balance task performance after 4 weeks of intrinsic-foot-muscle training: the short-foot exercise versus the towel-curl exercise. J Sport Rehabil. 2012. 21:327–33.
Article11.Rothermel SA., Hale SA., Hertel J., Denegar CR. Effect of active foot positioning on the outcome of a balance training program. Phys Ther Sport. 2004. 5:98–103.
Article12.Jung DY., Kim MH., Koh EK., Kwon OY., Cynn HS., Lee WH. A comparison in the muscle activity of the abductor hallucis and the medial longitudinal arch angle during toe curl and short foot exercises. Phys Ther Sport. 2011. 12:30–5.
Article13.Gray EG., Basmajian JV. Electromyography and cinematography of leg and foot ("normal" and flat) during walking. Anat Rec. 1968. 161:1–15.
Article14.Mann R., Inman VT. Phasic activity of intrinsic muscles of the foot. J Bone Joint Surg Am. 1964. 46:469–81.
Article15.Page P. Sensorimotor training: a “global” approach for balance training. J Bodyw Mov Ther. 2006. 10:77–84.
Article16.McKeon PO., Hertel J., Bramble D., Davis I. The foot core system: a new paradigm for understanding intrinsic foot muscle function. Br J Sports Med. 2015. 49:290.
Article17.Kalron A., Dvir Z., Frid L., Achiron A. Quantifying gait impairment using an instrumented treadmill in people with multiple sclerosis. ISRN Neurol. 2013. 2013:867575.18.Luessi F., Mueller LK., Breimhorst M., Vogt T. Influence of visual cues on gait in Parkinson's disease during treadmill walking at multiple velocities. J Neurol Sci. 2012. 314:78–82.
Article19.Bejek Z., Paroczai R., Illyes A., Kiss RM. The influence of walking speed on gait parameters in healthy people and in patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2006. 14:612–22.
Article20.Aminian A., Sangeorzan BJ. The anatomy of cavus foot deformity. Foot Ankle Clin. 2008. 13:191–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biomechanical Parameters in Plantar Fasciitis Measured by Gait Analysis System With Pressure Sensor
- Erratum: Biomechanical Parameters in Arch Building Gait Measured by Gait Analysis System with Pressure Sensor
- Insole Pressure Sensors to Assess Post-Stroke Gait
- Quantitative Analysis of Gait and Balance
- Effect of Ankle Foot Orthosis on Hemiplegic Gait