Korean J Ophthalmol.
2015 Feb;29(1):1-6. 10.3341/kjo.2015.29.1.1.
Dacryoscintigraphic Findings in the Children with Tearing
- Affiliations
-
- 1Department of Ophthalmology, Bundang CHA Hospital, CHA University, Seongnam, Korea. eye@cha.ac.kr
- 2Seoul St. Mary's Eye Hospital, Suwon, Korea.
- KMID: 2360131
- DOI: http://doi.org/10.3341/kjo.2015.29.1.1
Abstract
- PURPOSE
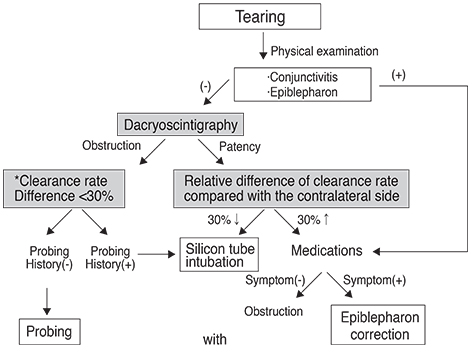
To investigate the diagnostic effectiveness of dacryoscintigraphy in children with tearing; to evaluate tear clearance rate as a diagnostic factor of dacryoscintigraphy in children with tearing; and to analyze the results of treatment according to dacryoscintigraphic findings in children with tearing.
METHODS
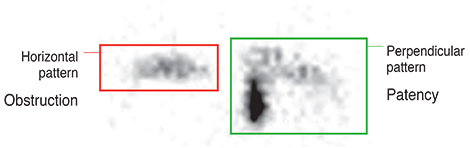
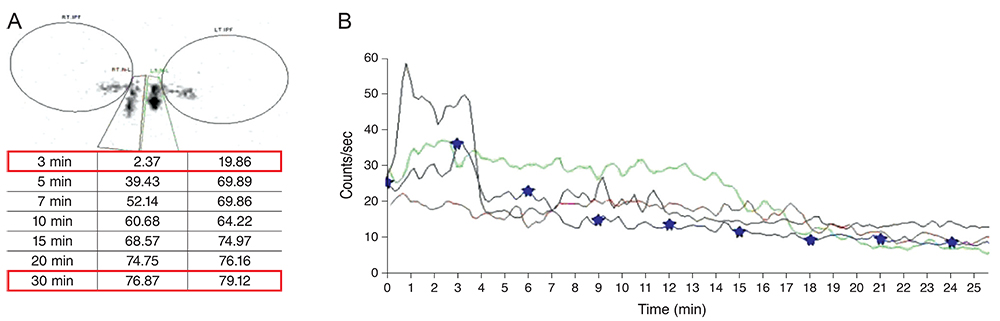
Between January 2010 and April 2014, 176 eyes of 88 children with tearing (49 boys and 39 girls; mean age, 23.81 ±14.67 months; range, 12 to 72 months) were studied retrospectively. Of these, 37 of 88 children with tearing were bilateral cases, and 51 were unilateral cases. None of the patients had a history of craniofacial disorder or trauma. The chief complaint of tearing with or without eye discharge and delivery mode, past history of neonatal conjunctivitis, syringing, or probing were collected from parents, grandparents, or previous hospital data. The drainage pattern of the nasolacrimal duct was analyzed, and the clearance rate of 50 microCi 99m technetium pertechnetate was measured by dacryoscintigraphy.
RESULTS
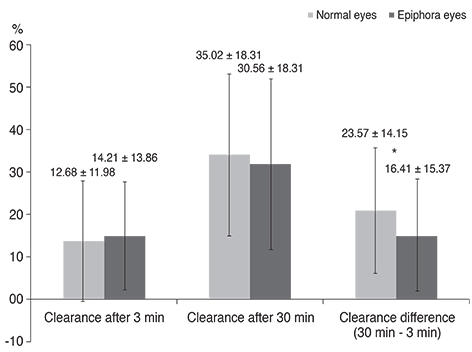
According to the dacryoscintigraphy results, 98 of 125 eyes (78.4%) with tearing showed nasolacrimal obstruction and 29 of 51 eyes (56.9%) without tearing showed patency. There was a significant difference between tearing eyes and normal eyes (p = 0.001). The clearance rate difference after 3 and 30 minutes was 16.41 ± 15.37% in tearing eyes and 23.57 ±14.15% in normal eyes. There was a significant difference between epiphoric eyes and normal eyes (p = 0.05). Based on the dacryoscintigraphic findings, nasolacrimal-duct obstruction was treated with probing or silicone-tube intubation. The majority of patients showed symptom improvement (75.2%) during the two months of follow-up.
CONCLUSIONS
Dacryoscintigraphy is a non-invasive method of qualitatively and quantitatively diagnosing nasolacrimal duct obstruction in children with tearing.
Keyword
MeSH Terms
Figure
Reference
-
1. Chung YA, Yoo IR, Oum JS, et al. The clinical value of dacryoscintigraphy in the selection of surgical approach for patients with functional lacrimal duct obstruction. Ann Nucl Med. 2005; 19:479–483.2. Schnall BM. Pediatric nasolacrimal duct obstruction. Curr Opin Ophthalmol. 2013; 24:421–424.3. Lorena SH, Silva JA, Scarpi MJ. Congenital nasolacrimal duct obstruction in premature children. J Pediatr Ophthalmol Strabismus. 2013; 50:239–244.4. Olitsky SE. Update on congenital nasolacrimal duct obstruction. Int Ophthalmol Clin. 2014; 54:1–7.5. Rossomondo RM, Carlton WH, Trueblood JH, Thomas RP. A new method of evaluating lacrimal drainage. Arch Ophthalmol. 1972; 88:523–525.6. Montanara A, Catalino P, Gualdi M. Improved radiological technique for evaluating the lacrimal pathways with special emphasis on functional disorders. Acta Ophthalmol. 1979; 57:547–563.7. Wearne MJ, Pitts J, Frank J, Rose GE. Comparison of dacryocystography and lacrimal scintigraphy in the diagnosis of functional nasolacrimal duct obstruction. Br J Ophthalmol. 1999; 83:1032–1035.8. Conway ST. Evaluation and management of "functional" nasolacrimal blockage: results of a survey of the American Society of Ophthalmic Plastic and Reconstructive surgery. Ophthal Plast Reconstr Surg. 1994; 10:185–187.9. Rosenstock T, Hurwitz JJ. Functional obstruction of the lacrimal drainage passages. Can J Ophthalmol. 1982; 17:249–255.10. Chung WS, Park NG. Functional obstruction of the lacrimal draings system. J Korean Ophthalmol Soc. 1995; 36:1435–1438.11. Shin CH, Woo KI, Chang HR. Evaluation of the functional nasolacrimal duct obstruction with digital subtraction dacryocystography. J Korean Ophthalmol Soc. 2003; 44:529–533.12. Chavis RM, Welham RA, Maisey MN. Quantitative lacrimal scintillography. Arch Ophthalmol. 1978; 96:2066–2068.13. Amanat LA, Hilditch TE, Kwok CS. Lacrimal scintigraphy. II. Its role in the diagnosis of epiphora. Br J Ophthalmol. 1983; 67:720–728.14. Hanna IT, MacEwen CJ, Kennedy N. Lacrimal scintigraphy in the diagnosis of epiphora. Nucl Med Commun. 1992; 13:416–420.15. Ziccardi VB, Charron M, Ochs MW, Braun TW. Nuclear dacryoscintigraphy: its role in oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:645–649.16. Sahlin S, Chen E. Gravity, blink rate, and lacrimal drainage capacity. Am J Ophthalmol. 1997; 124:758–764.17. Gencoglu EA, Dursun D, Akova YA, et al. Tear clearance measurement in patients with dry eye syndrome using quantitative lacrimal scintigraphy. Ann Nucl Med. 2005; 19:581–587.18. Park DI, Shin HM, Lee SY, Lew H. Tear production and drainage after botulinum toxin A injection in patients with essential blepharospasm. Acta Ophthalmol. 2013; 91:e108–e112.19. Miller AM, Chandler DL, Repka MX, et al. Office probing for treatment of nasolacrimal duct obstruction in infants. J AAPOS. 2014; 18:26–30.20. Alanon-Fernandez MA, Alanon-Fernandez FJ, Martinez-Fernandez A, et al. Comparative study of primary intention lacrimal probing with and without nasal endoscopy. Acta Otorrinolaringol Esp. 2014; 65:297–301.21. Angrist RC, Dortzbach RK. Silicone intubation for partial and total nasolacrimal duct obstruction in adults. Ophthal Plast Reconstr Surg. 1985; 1:51–54.22. Katowitz J, Hollsten D, Linberg J. Silicone intubation of the nasolacrimal drainage system. Lacrimal Surg. 1988; 109–123.23. Huh D, Son MG, Kim YD. Silicone intubation for functional nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2000; 41:2303–2307.24. Memon MN, Siddiqui SN, Arshad M, Altaf S. Nasolacrimal duct obstruction in children: outcome of primary intubation. J Pak Med Assoc. 2012; 62:1329–1332.25. Welsh MG, Katowitz JA. Timing of Silastic tubing removal after intubation for congenital nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 1989; 5:43–48.26. Heyman S, Katowitz JA, Smoger B. Dacryoscintigraphy in children. Ophthalmic Surg. 1985; 16:703–709.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Loss of Reflex Tearing after Maxillary Orthognathic Surgery Case Report and Literature Review
- Acute Malocclusion Related to Posterior Disc Displacement According to Complete Disc Tearing: Two Case Reports
- Clinical Implication of Dacryoendoscopy in the Patients with Tearing: A Systematic Review
- Role of Dacryoscintigraphy in the Diagnosis and Treatment of Pediatric with Epiphora
- Etiology of Epiphora