Anesth Pain Med.
2016 Apr;11(2):201-206. 10.17085/apm.2016.11.2.201.
An analysis of consultations requested to a pain clinic
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Bucheon St. Mary's Hospital, The Catholic University of Korea, Bucheon, Korea. pauly@catholic.ac.kr
- KMID: 2358486
- DOI: http://doi.org/10.17085/apm.2016.11.2.201
Abstract
- BACKGROUND
The study investigated in detail the current status of the consultations requested in a pain clinic. We evaluated the characteristics of the consultations to determine the kind of contents requested, referring departments and factors including demographics, co-morbidities, previous medical problems, and the descriptions of the reasons for the consultation to the pain clinic.
METHODS
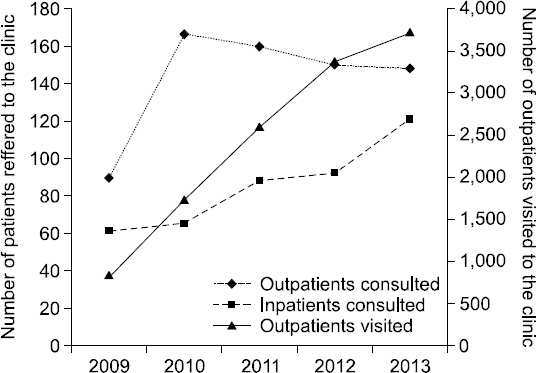
Clinical data were collected in the authors' institution between 1 January 2009 and 31 December 2013. The medical records were reviewed and compared. Characteristics of both outpatients and inpatients were analysed.
RESULTS
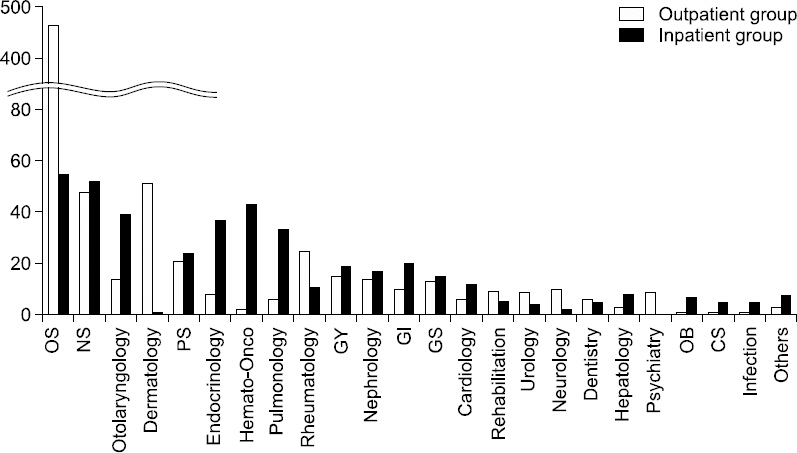
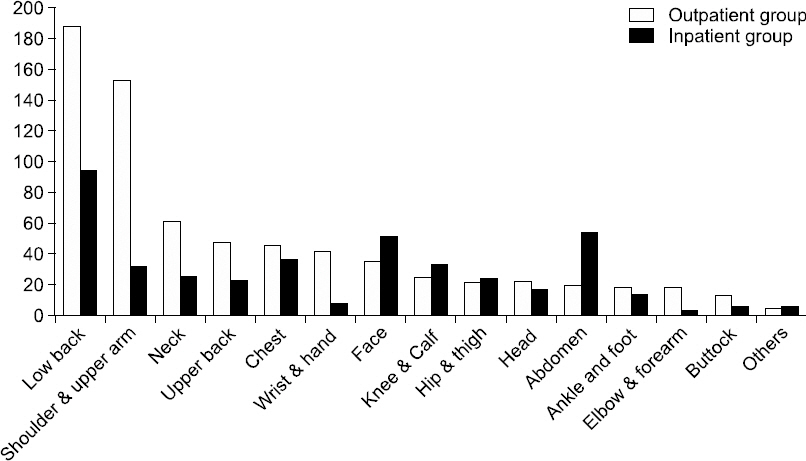
Data from 1,140 patients was available for this study. Seven hundred thirteen individuals belonged to the outpatient group and 427 individuals belonged to the inpatient group. Orthopedic surgery, neurosurgery, and otolaryngology were the main departments that requested consultations to the pain clinic. The most frequent requested lesion and diagnostic term were low back and lumbar spinal stenosis, respectively, and the most common reason for consulting was for "control of pain not controlled by medications." Factors that were significantly different between the two groups were gender, questions about other illnesses apart from the main diagnoses, history of specific diseases, acute onset, cancer, operation within 3 months, and physical system abnormalities.
CONCLUSIONS
The medical problems addressed by a pain clinic consultation service were diverse. It is rational to develop standardized guidelines for pain consultations, and treatment strategies aimed at alleviating pain per se as well as caring for comorbid conditions.
Keyword
MeSH Terms
Figure
Reference
-
1. Caputo GM, Gross RJ. Gross RJ, Caputo GM, editors. Function of a general internal medicine consultation service. Kammer and Gross’ Medical Consultation. 1998. 3rd ed. Baltimore: Williams & Wilkins;p. 9–18.2. Son SO. The approaches to postoperative pain management. J Korean Pain Soc. 1995; 8:1–7.3. Niv D, Devor M. Position paper of the European Federation of IASP Chapters (EFIC) on the subject of pain management. Eur J Pain. 2007; 11:487–9. DOI: 10.1016/j.ejpain.2007.03.005. PMID: 17433738.
Article4. Seo CM, Mun CW, Baek UY, Hong JG. A survey of patients visiting pain clinic. J Korean Pain Soc. 2000; 13:224–31.5. Nicholson B, Verma S. Comorbidities in chronic neuropathic pain. Pain Med. 2004; 5:S1–27. DOI: 10.1111/j.1526-4637.2004.04019.x.
Article6. Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain disability exaggeration/malingering and submaximal effort research. Clin J Pain. 1999; 15:244–74. DOI: 10.1097/00002508-199912000-00002. PMID: 10617254.
Article7. Davies HT, Crombie IK, Macrae WA, Rogers KM. Pain clinic patients in northern Britain. The Pain Clinic. 1991; 5:129–35.8. Choe H, Oh KH, Song JJ, Han YJ. Pain clinic 10 years at Chonbuk national university. J Korean Pain Soc. 1995; 8:110–6.9. Lim KI, Kim BK, Sohn HS. A clinical survey of the patients of pain clinic. J Korean Pain Soc. 1998; 11:288–93.10. Jang YH, Lee JK, Cheun JK, Chung JK. A clinical survey of paients of pain clinic. J Korean Pain Soc. 1995; 8:103–9.11. Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain. 1993; 9:174–82. DOI: 10.1097/00002508-199309000-00004. PMID: 8219517.12. Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007; 57:656–65. DOI: 10.1002/art.22684. PMID: 17471542.
Article13. Shin SH, Chung YP, Lim JJ, Yoon KB, Kim C. A clinical survey of patients of neuro-pain clinic. J Korean Pain Soc. 1994; 7:84–7.14. Shiotani M. Nerve blocking techniques for pain clinic. J Korean Pain Soc. 1992; 5:1–8.15. Hicks F, Simpson KH. Nerve blocks in palliative care. 2004. Oxford: Oxford university press;p. 33–41. DOI: 10.1093/acprof:oso/9780198527039.001.0001. PMID: 15163007.16. Kumar A. Organization and development of pain clinics and palliative care in developing countries. Eur J Anaesthesiol. 2004; 21:169–72. DOI: 10.1097/00003643-200403000-00001. PMID: 15055887.
Article17. Gallagher RM, Rauh V, Haugh LD, Milhous R, Callas PW, Langelier R, et al. Determinants of return-to-work among low back pain patients. Pain. 1989; 39:55–67. DOI: 10.1016/0304-3959(89)90175-9.
Article18. van Wilgen CP, Keizer D. Neuropathic pain mechanisms in patients with chronic sports injuries: a diagnostic model useful in sports medicine? Pain Med. 2011; 12:110–7. DOI: 10.1111/j.1526-4637.2010.01023.x. PMID: 21143763.
Article19. Koop SM, ten Klooster PM, Vonkeman HE, Steunebrink LM, van de Laar MA. Neuropathic-like pain features and cross-sectional associations in rheumatoid arthritis. Arthritis Res Ther. 2015; 17:237. DOI: 10.1186/s13075-015-0761-8. PMID: 26335941. PMCID: PMC4558794.
Article20. Fitzcharles MA, Almahrezi A, Ware MA. Clinical profile of rheumatic disease patients referred to a multidisciplinary pain center. J Rheumatol. 2004; 31:359–63. PMID: 14760809.21. Marks JL, Colebatch AN, Buchbinder R, Edwards CJ. Pain management for rheumatoid arthritis and cardiovascular or renal comorbidity. Cochrane Database Syst Rev. 2011; 10:CD008952. DOI: 10.1002/14651858.cd008952.pub2.
Article22. Radner H, Ramiro S, van der Heijde DM, Landewé R, Buchbinder R, Aletaha D. How do gastrointestinal or liver comorbidities influence the choice of pain treatment in inflammatory arthritis? A Cochrane systematic review. J Rheumatol Suppl. 2012; 90:74–80. DOI: 10.3899/jrheum.120346. PMID: 22942333.
Article23. Ramiro S, Radner H, van der Heijde D, van Tubergen A, Buchbinder R, Aletaha D, et al. Combination therapy for pain management in inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, other spondyloarthritis). Cochrane Database Syst Rev. 2011; 10:CD008886. DOI: 10.1002/14651858.cd008886.pub2.
Article24. Romano JM, Turner JA. Chronic pain and depression: does the evidence support a relationship? Psychol Bull. 1985; 97:18–34. DOI: 10.1037/0033-2909.97.1.18. PMID: 3983297.
Article25. Pupa LE Jr, Coventry JA, Hanley JF, Carpenter JL. Factors affecting compliance for general medicine consultations to non-internists. Am J Med. 1986; 81:508–14. DOI: 10.1016/0002-9343(86)90307-4.
Article26. Searle RD, Howell SJ, Bennett MI. Diagnosing postoperative neuropathic pain: a Delphi survey. Br J Anaesth. 2012; 109:240–4. DOI: 10.1093/bja/aes147. PMID: 22649184.
Article27. Miaskowski C, Crews J, Ready LB, Paul SM, Ginsberg B. Anesthesia-based pain services improve the quality of postoperative pain management. Pain. 1999; 80:23–9. DOI: 10.1016/S0304-3959(98)00192-4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Interdepartmental Consultation (2)
- Analysis of Medical Consultation Patterns in Medical and Surgical Intensive Care Units: Changes in the Pattern of Consultation after the Implementation of Intensivist-Directed Care
- A Statistical Analysis of the Patients in Anesthesia Preoperative Evaluation Clinic
- Changing Guidelines for Clinical Microbiology Laboratories and Their Influences on Workflows Related to Consultations
- The Pain Alterations in Terminal Cancer Patients Who Received Pain Control