Brain Tumor Res Treat.
2016 Oct;4(2):128-132. 10.14791/btrt.2016.4.2.128.
Metastatic Intracranial Hemangiopericytoma to the Spinal Column: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Konkuk University Medical Center, Seoul, Korea. kohyc@kuh.ac.kr
- 2Department of Radiology, Konkuk University Medical Center, Seoul, Korea.
- 3Department of Pathology, Konkuk University Medical Center, Seoul, Korea.
- KMID: 2356982
- DOI: http://doi.org/10.14791/btrt.2016.4.2.128
Abstract
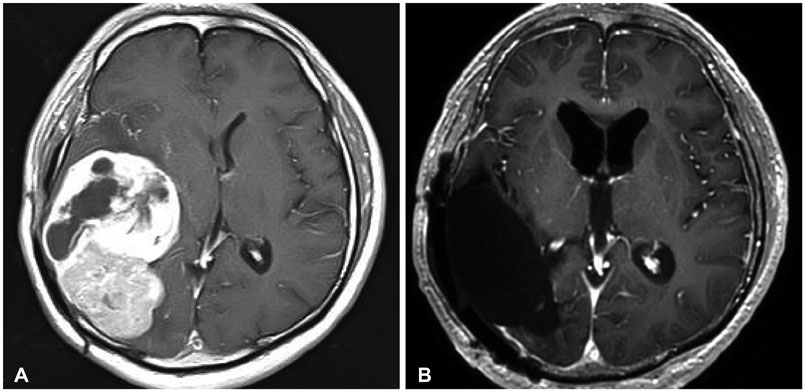
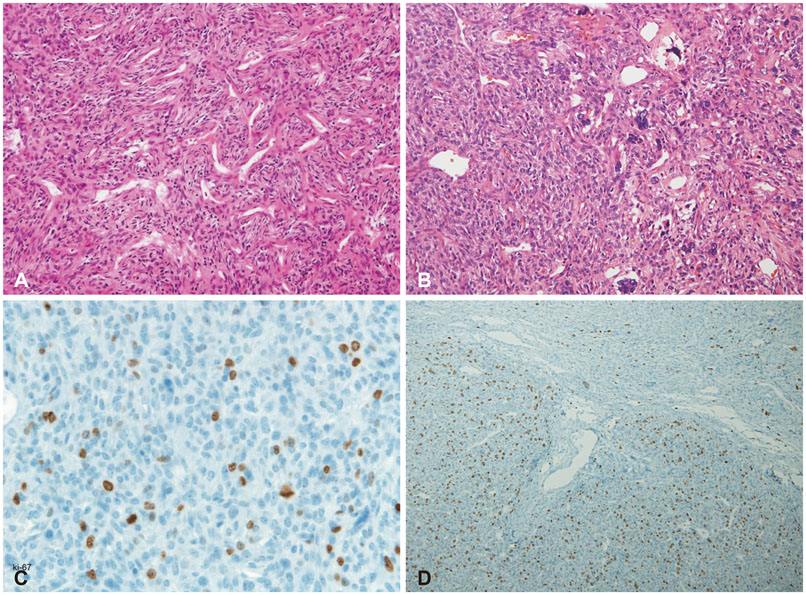
- Intracranial hemangiopericytoma (HPC) is a rare brain tumor with aggressive biologic behavior associated with high recurrence rate and often with extracranial metastasis. The most common sites of extracranial metastasis of the intracranial HPC are the long bones, lung, liver and abdominal cavity in the order of frequencies. Extracranial metastases usually occur long after the initial diagnosis of the primary tumor. Metastatic intracranial HPC to the vertebra has been rarely reported. We present a case of intracranial HPC metastasized to the L2 vertebral body 13 years after multiple surgical resections and radiotherapy of the primary intracranial HPC.
Keyword
MeSH Terms
Figure
Reference
-
1. Fredriksson F, Nordborg C, Hallén T, Blomquist E. Haemangiopericytoma presenting with acute intracerebral haemorrhage--a case report and literature review. Acta Oncol. 2013; 52:753–758.
Article2. Dufour H, Métellus P, Fuentes S, et al. Meningeal hemangiopericytoma: a retrospective study of 21 patients with special review of postoperative external radiotherapy. Neurosurgery. 2001; 48:756–762. discussion 762-3.
Article3. Thomas HG, Dolman CL, Berry K. Malignant meningioma: clinical and pathological features. J Neurosurg. 1981; 55:929–934.
Article4. Thompson L. World Health Organization classification of tumours: pathology and genetics of head and neck tumours. Ear Nose Throat J. 2006; 85:74.
Article5. Soyuer S, Chang EL, Selek U, McCutcheon IE, Maor MH. Intracranial meningeal hemangiopericytoma: the role of radiotherapy: report of 29 cases and review of the literature. Cancer. 2004; 100:1491–1497.
Article6. Woitzik J, Sommer C, Krauss JK. Delayed manifestation of spinal metastasis: a special feature of hemangiopericytoma. Clin Neurol Neurosurg. 2003; 105:159–166.
Article7. Guthrie BL, Ebersold MJ, Scheithauer BW, Shaw EG. Meningeal hemangiopericytoma: histopathological features, treatment, and long-term follow-up of 44 cases. Neurosurgery. 1989; 25:514–522.
Article8. Lee JK, Kim SH, Joo SP, et al. Spinal metastasis from cranial meningeal hemangiopericytomas. Acta Neurochir (Wien). 2006; 148:787–790.
Article9. Batson OV. The function of the vertebral veins and their role in the spread of metastases. 1940. Clin Orthop Relat Res. 1995; (312):4–9.10. Batson OV. The vertebral vein system. Caldwell lecture, 1956. Am J Roentgenol Radium Ther Nucl Med. 1957; 78:195–212.11. Cappuccio M, Gasbarrini A, Van Urk P, Bandiera S, Boriani S. Spinal metastasis: a retrospective study validating the treatment algorithm. Eur Rev Med Pharmacol Sci. 2008; 12:155–160.12. Arguello F, Baggs RB, Duerst RE, Johnstone L, McQueen K, Frantz CN. Pathogenesis of vertebral metastasis and epidural spinal cord compression. Cancer. 1990; 65:98–106.
Article13. Lugassy C, Zadran S, Bentolila LA, et al. Angiotropism, pericytic mimicry and extravascular migratory metastasis in melanoma: an alternative to intravascular cancer dissemination. Cancer Microenviron. 2014; 7:139–152.
Article14. Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109.
Article15. Nonaka M, Kohmura E, Hirata M, Hayakawa T. Metastatic meningeal hemangiopericytoma of thoracic spine. Clin Neurol Neurosurg. 1998; 100:228–230.
Article16. Alawi F, Stratton D, Freedman PD. Solitary fibrous tumor of the oral soft tissues: a clinicopathologic and immunohistochemical study of 16 cases. Am J Surg Pathol. 2001; 25:900–910.17. Robinson DR, Wu YM, Kalyana-Sundaram S, et al. Identification of recurrent NAB2-STAT6 gene fusions in solitary fibrous tumor by integrative sequencing. Nat Genet. 2013; 45:180–185.
Article18. Mena H, Ribas JL, Pezeshkpour GH, Cowan DN, Parisi JE. Hemangiopericytoma of the central nervous system: a review of 94 cases. Hum Pathol. 1991; 22:84–91.
Article19. Kruse F Jr. Hemangiopericytoma of the meniges (angioblastic meningioma of Cushing and Eisenhardt). Clinico-pathologic aspects and follow-up studies in 8 cases. Neurology. 1961; 11:771–777.
Article20. Scott M, Kellett G, Peale A. Angioblastic meningioma (hemangiopericytoma) of the cerebellar fossa with metastases to the temporal bone and the lumbar spine. Surg Neurol. 1974; 2:35–38.21. Taniura S, Taniguchi M, Mizutani T, Takahashi H. Metastatic hemangiopericytoma to the cauda equina: a case report. Spine J. 2007; 7:371–373.
Article22. Cole CD, Schmidt MH. Hemangiopericytomas of the spine: case report and review of the literature. Rare Tumors. 2009; 1:e43.
Article23. Fukuda Y, Watanabe K, Toyama Y, Mikami S, Matsumoto M. Metastasis of intracranial meningeal hemangiopericytoma to thoracic spine 17 years after surgical excision: a case report. J Orthop Sci. 2015; 20:425–429.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Rare Case of Cerebral Metastasis from Hemangiopericytoma in Pelvis
- Hemangiopericyotma with Metastasis to the Cervical Spine: Case Report
- Multiple Spinal Metastases of Hemangiopericytoma: Case Report
- Metastatic Pulmonary Hemangiopericytoma from Retroperitoneum: A case report
- Metastatic Hemangiopericytoma of the Liver: A Case Report