Ann Surg Treat Res.
2016 Nov;91(5):239-246. 10.4174/astr.2016.91.5.239.
Prevalence and characteristics of clinically significant retained common bile duct stones after laparoscopic cholecystectomy for symptomatic cholelithiasis
- Affiliations
-
- 1Department of Surgery, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea. ahndori68@naver.com
- KMID: 2356374
- DOI: http://doi.org/10.4174/astr.2016.91.5.239
Abstract
- PURPOSE
To investigate the prevalence and clinical features of retained symptomatic common bile duct (CBD) stone detected after laparoscopic cholecystectomy (LC) in patients without preoperative evidence of CBD or intrahepatic duct stones.
METHODS
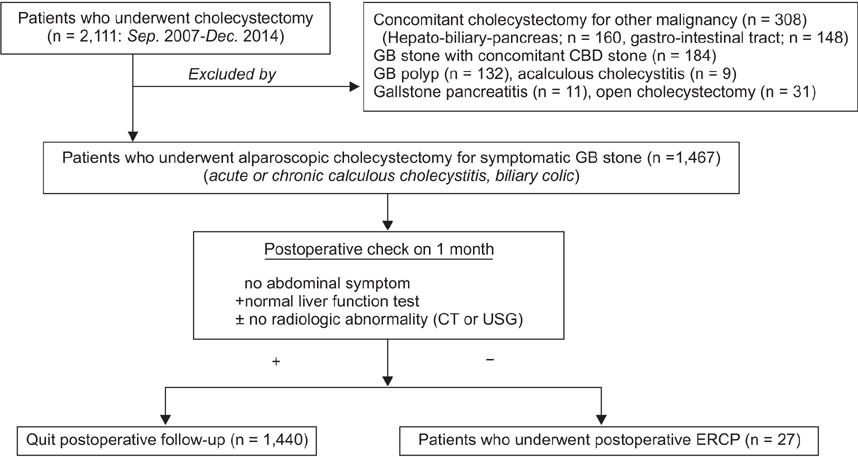
Of 2,111 patients who underwent cholecystectomy between September 2007 and December 2014 at Seoul Metropolitan Government-Seoul National University Boramae Medical Center, 1,467 underwent laparoscopic cholecystectomy for symptomatic gallbladder stones and their medical records were analyzed. We reviewed the clinical data of patients who underwent postoperative endoscopic retrograde cholangiopancreatography (ERCP) for clinically significant CBD stones (i.e., symptomatic stones requiring therapeutic intervention).
RESULTS
Overall, 27 of 1,467 patients (1.84%) underwent postoperative ERCP after LC because of clinical evidence of retained CBD stones. The median time from LC to ERCP was 152 days (range, 60-1,015 days). Nine patients had ERCP-related complications. The median hospital stay for ERCP was 6 days.
CONCLUSION
The prevalence of clinically significant retained CBD stone after LC for symptomatic cholelithiasis was 1.84% and the time from LC to clinical presentation ranged from 2 months to 2 years 9 months. Therefore, biliary surgeons should inform patients that retained CBD stone may be detected several years after LC for simple gallbladder stones.
Keyword
MeSH Terms
Figure
Reference
-
1. Bhat M, Romagnuolo J, da Silveira E, Reinhold C, Valois E, Martel M, et al. Randomised clinical trial: MRCP-first vs. ERCP-first approach in patients with suspected biliary obstruction due to bile duct stones. Aliment Pharmacol Ther. 2013; 38:1045–1053.2. Morris S, Gurusamy KS, Sheringham J, Davidson BR. Cost-effectiveness analysis of endoscopic ultrasound versus magnetic resonance cholangiopancreatography in patients with suspected common bile duct stones. PLoS One. 2015; 10:e0121699.3. Peng WK, Sheikh Z, Paterson-Brown S, Nixon SJ. Role of liver function tests in predicting common bile duct stones in acute calculous cholecystitis. Br J Surg. 2005; 92:1241–1247.4. Nickkholgh A, Soltaniyekta S, Kalbasi H. Routine versus selective intraoperative cholangiography during laparoscopic cholecystectomy: a survey of 2,130 patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2006; 20:868–874.5. Stuart SA, Simpson TI, Alvord LA, Williams MD. Routine intraoperative laparoscopic cholangiography. Am J Surg. 1998; 176:632–637.6. Collins C, Maguire D, Ireland A, Fitzgerald E, O'Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg. 2004; 239:28–33.7. Randial Perez LJ, Fernando Parra J, Aldana Dimas G. The safety of early laparoscopic cholecystectomy (<48 hours) for patients with mild gallstone pancreatitis: a systematic review of the literature and meta-analysis. Cir Esp. 2014; 92:107–113.8. Dawe SR, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ. A systematic review of surgical skills transfer after simulation-based training: laparoscopic cholecystectomy and endoscopy. Ann Surg. 2014; 259:236–248.9. Lee SC, Choi BJ, Kim SJ. Two-port cholecystectomy maintains safety and feasibility in benign gallbladder diseases: a comparative study. Int J Surg. 2014; 12:1014–1019.10. Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, et al. Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 2015; 18:196–204.11. Kullman E, Borch K, Lindstrom E, Svanvik J, Anderberg B. Value of routine intraoperative cholangiography in detecting aberrant bile ducts and bile duct injuries during laparoscopic cholecystectomy. Br J Surg. 1996; 83:171–175.12. Nebiker CA, Baierlein SA, Beck S, von Flue M, Ackermann C, Peterli R. Is routine MR cholangiopancreatography (MRCP) justified prior to cholecystectomy? Langenbecks Arch Surg. 2009; 394:1005–1010.13. Suzuki N, Takahashi W, Sato T. Types and chemical composition of intrahepatic stones. Prog Clin Biol Res. 1984; 152:71–80.14. Kaufman HS, Magnuson TH, Lillemoe KD, Frasca P, Pitt HA. The role of bacteria in gallbladder and common duct stone formation. Ann Surg. 1989; 209:584–591.15. Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol. 2006; 20:1075–1083.16. Bonatsos G, Leandros E, Dourakis N, Birbas C, Delibaltadakis G, Golematis B. Laparoscopic cholecystectomy. Intraoperative findings and postoperative complications. Surg Endosc. 1995; 9:889–893.17. Dexter SP, Martin IG, Marton J, McMahon MJ. Long operation and the risk of complications from laparoscopic cholecystectomy. Br J Surg. 1997; 84:464–466.18. Saharia PC, Zuidema GD, Cameron JL. Primary common duct stones. Ann Surg. 1977; 185:598–604.19. Kim BS, Joo SH, Cho S, Han MS. Who experiences endoscopic retrograde cholangiopancreatography after laparoscopic cholecystectomy for symptomatic gallstone disease? Ann Surg Treat Res. 2016; 90:309–314.20. Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005; 54:271–275.21. Okada M, Fukada J, Toya K, Ito R, Ohashi T, Yorozu A. The value of drip infusion cholangiography using multidetector-row helical CT in patients with choledocholithiasis. Eur Radiol. 2005; 15:2140–2145.22. Ammori BJ, Birbas K, Davides D, Vezakis A, Larvin M, McMahon MJ. Routine vs "on demand" postoperative ERCP for small bile duct calculi detected at intraoperative cholangiography. Clinical evaluation and cost analysis. Surg Endosc. 2000; 14:1123–1126.23. Horwood J, Akbar F, Davis K, Morgan R. Prospective evaluation of a selective approach to cholangiography for suspected common bile duct stones. Ann R Coll Surg Engl. 2010; 92:206–210.24. Brown LM, Rogers SJ, Cello JP, Brasel KJ, Inadomi JM. Cost-effective treatment of patients with symptomatic cholelithiasis and possible common bile duct stones. J Am Coll Surg. 2011; 212:1049–1060. 1060.e1–1060.e7.25. Ding GQ, Cai W, Qin MF. Is intraoperative cholangiography necessary during laparoscopic cholecystectomy for cholelithiasis? World J Gastroenterol. 2015; 21:2147–2151.26. Bahram M, Gaballa G. The value of preoperative magnetic resonance cholangiopancreatography (MRCP) in management of patients with gall stones. Int J Surg. 2010; 8:342–345.27. Epelboym I, Winner M, Allendorf JD. MRCP is not a cost-effective strategy in the management of silent common bile duct stones. J Gastrointest Surg. 2013; 17:863–871.28. Videhult P, Sandblom G, Rudberg C, Rasmussen IC. Are liver function tests, pancreatitis and cholecystitis predictors of common bile duct stones? Results of a prospective, population-based, cohort study of 1171 patients undergoing cholecystectomy. HPB (Oxford). 2011; 13:519–527.29. Cox MR, Budge JP, Eslick GD. Timing and nature of presentation of unsuspected retained common bile duct stones after laparoscopic cholecystectomy: a retrospective study. Surg Endosc. 2015; 29:2033–2038.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic cholecystectomy and common bile duct exploration for gallstone and common bile duct stone in a patient with a left-sided gallbladder: a case report
- Clinical Review of the Management of Cholelithiasis & Choledocholithiasis
- Clinical Analysis of Laparoscopic Cholecystectomy in Complicated Cholelithiasis
- Surgical Clip Moved into the Extrahepatic Bile Duct after Laparoscopic Hepatectomy
- Laparoscopic Surgery for Common Bile Duct Stone