Clin Endosc.
2016 Sep;49(5):434-437. 10.5946/ce.2016.127.
Endoscopic Submucosal Dissection for Early Gastric Cancers with Uncommon Histology
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. doc0224@pusan.ac.kr
- KMID: 2356048
- DOI: http://doi.org/10.5946/ce.2016.127
Abstract
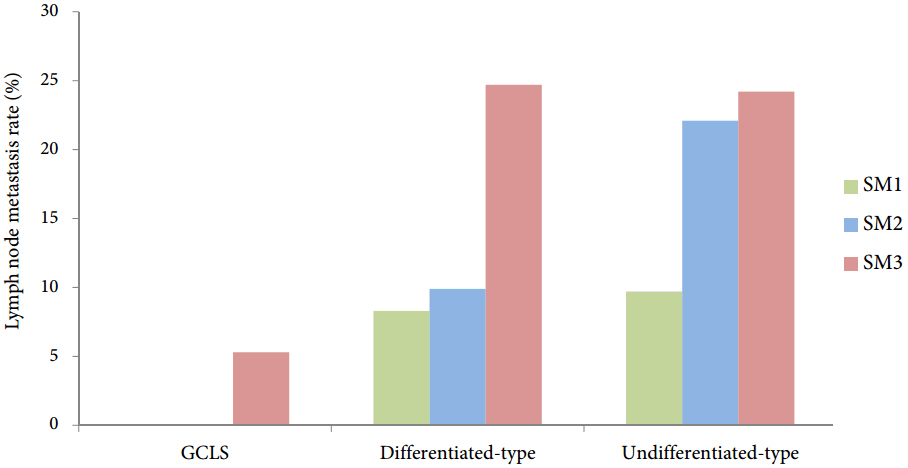
- Endoscopic submucosal dissection (ESD) enables en bloc curative resection of early gastric cancers (EGCs) with a negligible risk of lymph node metastasis (LNM). Although ESD for EGCs with absolute and expanded indications is safe, the results differ between EGCs with specialized and common histologies. EGC with papillary adenocarcinoma is a differentiated-type adenocarcinoma. At present, it is treated with ESD according to the same criteria as other differentiated-type adenocarcinomas. The LNM rate under the current indication criteria is high, and over half of the patients who undergo ESD as a primary treatment for EGC with papillary adenocarcinoma achieve an out-of-ESD result. Gastric carcinoma with lymphoid stroma in EGC has a low LNM rate and a favorable outcome, despite deep submucosal invasion. Patients with this gastric cancer subtype may be good candidates for ESD, even with deep submucosal invasion. Large-scale prospective multi-center studies with longer follow-up periods are needed to set proper ESD criteria for these tumors. Clinicians should be aware of these disease entities and ESD should be more carefully considered for EGCs with papillary adenocarcinoma and gastric carcinoma with lymphoid stroma.
MeSH Terms
Figure
Cited by 1 articles
-
Pitfalls in the Interpretation of Publications about Endoscopic Submucosal Dissection of Early Gastric Cancer with Undifferentiated-Type Histology
Chang Seok Bang, Gwang Ho Baik
Clin Endosc. 2019;52(1):30-35. doi: 10.5946/ce.2018.158.
Reference
-
1. Abe N, Gotoda T, Hirasawa T, et al. Multicenter study of the long-term outcomes of endoscopic submucosal dissection for early gastric cancer in patients 80 years of age or older. Gastric Cancer. 2012; 15:70–75.2. Choi MK, Kim GH, Park DY, et al. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a single-center experience. Surg Endosc. 2013; 27:4250–4258.
Article3. Abe S, Oda I, Suzuki H, et al. Short- and long-term outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Endoscopy. 2013; 45:703–707.
Article4. Chung IK, Lee JH, Lee SH, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009; 69:1228–1235.
Article5. Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000; 3:219–225.
Article6. Hu B, El Hajj N, Sittler S, Lammert N, Barnes R, Meloni-Ehrig A. Gastric cancer: classification, histology and application of molecular pathology. J Gastrointest Oncol. 2012; 3:251–261.7. Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965; 64:31–49.8. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.9. Yasuda K, Adachi Y, Shiraishi N, Maeo S, Kitano S. Papillary adenocarcinoma of the stomach. Gastric Cancer. 2000; 3:33–38.
Article10. Takizawa K, Ono H, Kakushima N, et al. Risk of lymph node metastases from intramucosal gastric cancer in relation to histological types: how to manage the mixed histological type for endoscopic submucosal dissection. Gastric Cancer. 2013; 16:531–536.
Article11. Hanaoka N, Tanabe S, Mikami T, Okayasu I, Saigenji K. Mixed-histologic-type submucosal invasive gastric cancer as a risk factor for lymph node metastasis: feasibility of endoscopic submucosal dissection. Endoscopy. 2009; 41:427–432.
Article12. Okada K, Fujisaki J, Yoshida T, et al. Long-term outcomes of endoscopic submucosal dissection for undifferentiated-type early gastric cancer. Endoscopy. 2012; 44:122–127.
Article13. Lee HJ, Kim GH, Park DY, et al. Is endoscopic submucosal dissection safe for papillary adenocarcinoma of the stomach? World J Gastroenterol. 2015; 21:3944–3952.
Article14. Akagi T, Shiraishi N, Kitano S. Lymph node metastasis of gastric cancer. Cancers (Basel). 2011; 3:2141–2159.
Article15. Noh H, Park JJ, Yun JW, et al. Clinicopathologic characteristics of patients who underwent curative additional gastrectomy after endoscopic submucosal dissection for early gastric cancer or adenoma. Korean J Gastroenterol. 2012; 59:289–295.
Article16. Jung H, Bae JM, Choi MG, Noh JH, Sohn TS, Kim S. Surgical outcome after incomplete endoscopic submucosal dissection of gastric cancer. Br J Surg. 2011; 98:73–78.
Article17. Lauwers GY, Carneiro F, Graham DY, et al. Gastric carcinoma. In : Bosman FT, Carneiro F, Hruban RH, editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research against Cancer;2010. p. 48–58.18. Lee JH, Kim SH, Han SH, An JS, Lee ES, Kim YS. Clinicopathological and molecular characteristics of Epstein-Barr virus-associated gastric carcinoma: a meta-analysis. J Gastroenterol Hepatol. 2009; 24:354–365.
Article19. Lee HE, Chae SW, Lee YJ, et al. Prognostic implications of type and density of tumour-infiltrating lymphocytes in gastric cancer. Br J Cancer. 2008; 99:1704–1711.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Submucosal Dissection in the Treatment of Patients With Papillary Early Gastric Cancer
- The Histologic Discrepancy before and after Endoscopic Submucosal Dissection of Gastric Adenoma and Early Gastric Cancer
- Future Development of Endoscopic Accessories for Endoscopic Submucosal Dissection
- Endoscopic Treatment for Early Gastric Cancer
- Pathological Interpretation of Gastric Tumors in Endoscopic Submucosal Dissection