J Cerebrovasc Endovasc Neurosurg.
2016 Sep;18(3):306-314. 10.7461/jcen.2016.18.3.306.
Recurrent Carotid Cavernous Fistula Originating from a Giant Cerebral Aneurysm after Placement of a Covered Stent
- Affiliations
-
- 1Department of Neurosurgery, Busan Paik Hospital, Inje University, School of Medicine, Busan, Korea. kimst015@hanmail.net
- 2Department of Diagnostic Radiology, Busan Paik Hospital, Inje University, School of Medicine, Busan, Korea.
- 3Department of Neurology, Busan Paik Hospital, Inje University, School of Medicine, Busan, Korea.
- KMID: 2355660
- DOI: http://doi.org/10.7461/jcen.2016.18.3.306
Abstract
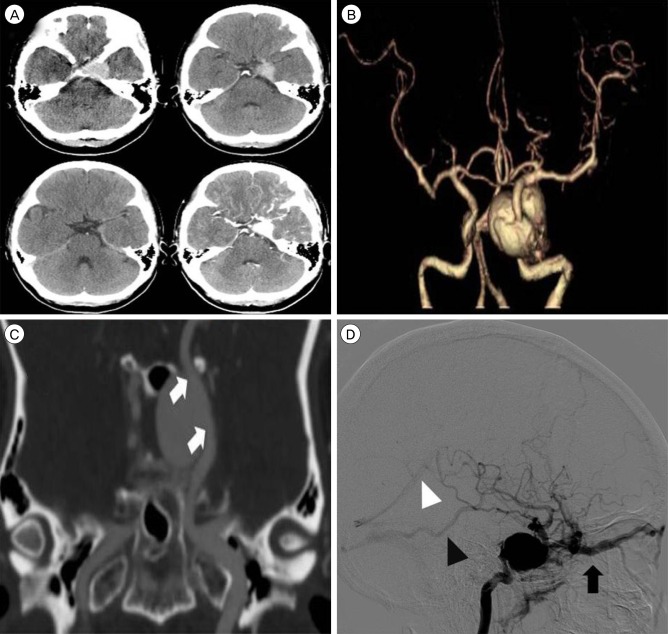
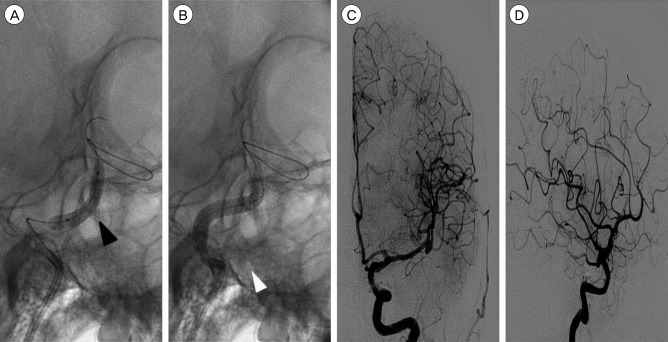
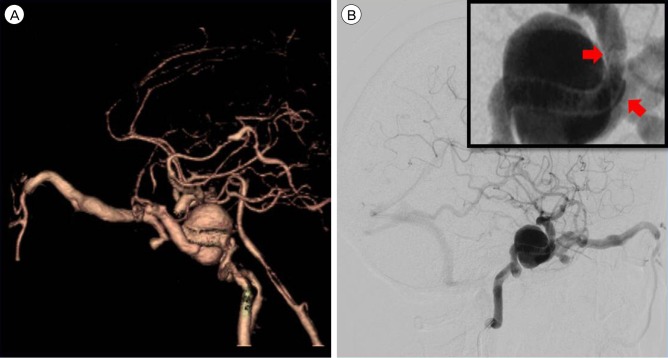
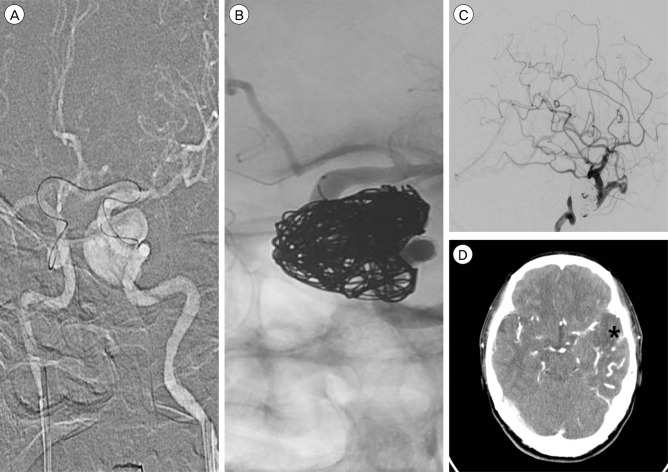
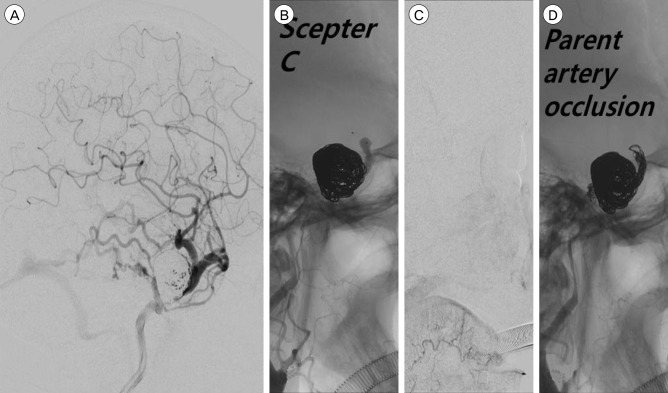
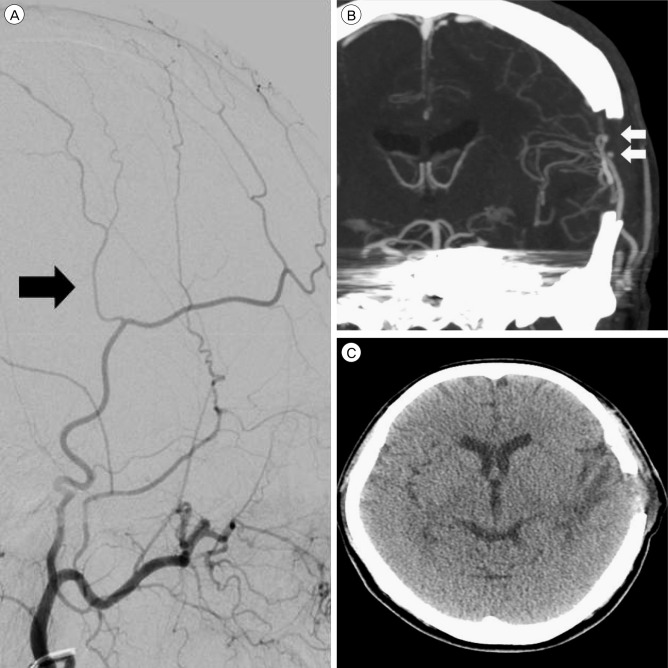
- We report the case of a recurrent carotid cavernous fistula (CCF) originating from a giant cerebral aneurysm (GCA) after placement of a covered stent. A 47-year-old woman presented with sudden onset of severe headache, and left-sided exophthalmos and ptosis. Cerebral angiography revealed a CCF caused by rupture of a GCA in the cavernous segment of the left internal carotid artery. Two covered stents were placed at the neck of the aneurysm. The neurological symptoms improved at first, but were aggravated in the 6 months following the treatment. Contrast agent endoleak was seen in the distal area of the stent. Even though additional treatments were attempted via an endovascular approach, the CCF could not be cured. However, after trapping the aneurysm using coils and performing superficial temporal artery-middle cerebral artery bypass, the neurological symptoms improved. In cases of recurrent CCF originating from a GCA after placement of a covered stent, it is possible to treat the CCF by endovascular trapping and surgical bypass.
MeSH Terms
Figure
Reference
-
1. Archondakis E, Pero G, Valvassori L, Boccardi E, Scialfa G. Angiographic follow-up of traumatic carotid cavernous fistulas treated with endovascular stent graft placement. AJNR Am J Neuroradiol. 2007; 2. 28(2):342–347. PMID: 17297009.2. Bonello L, Tantry US, Marcucci R, Blindt R, Angiolillo DJ, Becker R, et al. Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J Am Coll Cardiol. 2010; 9. 56(12):919–933. PMID: 20828644.
Article3. Delgado Almandoz JE, Crandall BM, Scholz JM, Fease JL, Anderson RE, Kadkhodayan Y, et al. Last-recorded P2Y12 reaction units value is strongly associated with thromboembolic and hemorrhagic complications occurring up to 6 months after treatment in patients with cerebral aneurysms treated with the pipeline embolization device. AJNR Am J Neuroradiol. 2014; 1. 35(1):128–135. PMID: 23828107.
Article4. Delgado Almandoz JE, Kadkhodayan Y, Crandall BM, Scholz JM, Fease JL, Tubman DE. Variability in initial response to standard clopidogrel therapy, delayed conversion to clopidogrel hyper-response, and associated thromboembolic and hemorrhagic complications in patients undergoing endovascular treatment of unruptured cerebral aneurysms. J Neurointerv Surg. 2014; 12. 6(10):767–773. PMID: 24353331.
Article5. dos Santos ML, Spotti AR, dos Santos RM, Borges MA, Ferrari AF, Colli BO, et al. Giant intracranial aneurysms: Morphology and clinical presentation. Neurosurg Rev. 2013; 1. 36(1):117–122. discussion 122. PMID: 22791075.
Article6. Eddleman CS, Surdell D, Miller J, Shaibani A, Bendok BR. Endovascular management of a ruptured cavernous carotid artery aneurysm associated with a carotid cavernous fistula with an intracranial self-expanding microstent and hydrogel-coated coil embolization: Case report and review of the literature. Surg Neurol. 2007; 11. 68(5):562–567. discussion 567. PMID: 17961748.
Article7. Geisler T, Zurn C, Simonenko R, Rapin M, Kraibooj H, Kilias A, et al. Early but not late stent thrombosis is influenced by residual platelet aggregation in patients undergoing coronary interventions. Eur Heart J. 2010; 1. 31(1):59–66. PMID: 19812059.
Article8. Gomez F, Escobar W, Gomez AM, Gomez JF, Anaya CA. Treatment of carotid cavernous fistulas using covered stents: Midterm results in seven patients. AJNR Am J Neuroradiol. 2007; 10. 28(9):1762–1768. PMID: 17885249.
Article9. Kobayashi N, Miyachi S, Negoro M, Suzuki O, Hattori K, Kojima T, et al. Endovascular treatment strategy for direct carotid-cavernous fistulas resulting from rupture of intracavernous carotid aneurysms. AJNR Am J Neuroradiol. 2003; 10. 24(9):1789–1796. PMID: 14561604.10. Kupersmith MJ, Hurst R, Berenstein A, Choi IS, Jafar J, Ransohoff J. The benign course of cavernous carotid artery aneurysms. J Neurosurg. 1992; 11. 77(5):690–693. PMID: 1403108.
Article11. Lewis AI, Tomsick TA, Tew JM Jr. Management of 100 consecutive direct carotid-cavernous fistulas: Results of treatment with detachable balloons. Neurosurgery. 1995; 2. 36(2):239–244. discussion 244-5. PMID: 7731502.12. Li K, Cho YD, Kim KM, Kang HS, Kim JE, Han MH. Covered stents for the endovascular treatment of a direct carotid cavernous fistula : Single center experiences with 10 cases. J Korean Neurosurg Soc. 2015; 1. 57(1):12–18. PMID: 25674338.
Article13. Polin RS, Shaffrey ME, Jensen ME, Braden L, Ferguson RD, Dion JE, et al. Medical management in the endovascular treatment of carotid-cavernous aneurysms. J Neurosurg. 1996; 5. 84:755–761. PMID: 8622148.
Article14. Sibbing D, Morath T, Braun S, Stegherr J, Mehilli J, Vogt W, et al. Clopidogrel response status assessed with multiplate point-of-care analysis and the incidence and timing of stent thrombosis over six months following coronary stenting. Thromb Haemost. 2010; 1. 103(1):151–159. PMID: 20062919.
Article15. Sugawara Y, Kikuchi T, Ueda T, Nishizaki M, Nakata S, Mochizuki T, et al. Usefulness of brain SPECT to evaluate brain tolerance and hemodynamic changes during temporary balloon occlusion test and after permanent carotid occlusion. J Nucl Med. 2002; 12. 43(12):1616–1623. PMID: 12468510.16. Tiewei Q, Ali A, Shaolei G, Feng L, Zhongsong S, Xuesong L, et al. Carotid cavernous fistulas treated by endovascular covered stent grafts with follow-up results. Br J Neurosurg. 2010; 8. 24(4):435–440. PMID: 20515263.
Article17. van Rooij WJ, Sluzewski M, Beute GN. Ruptured cavernous sinus aneurysms causing carotid cavernous fistula: Incidence, clinical presentation, treatment, and outcome. AJNR Am J Neuroradiol. 2006; 1. 27(1):185–189. PMID: 16418380.18. van Rooij WJ, Sluzewski M, Metz NH, Nijssen PC, Wijnalda D, Rinkel GJ, et al. Carotid balloon occlusion for large and giant aneurysms: Evaluation of a new test occlusion protocol. Neurosurgery. 2000; 7. 47(1):116–121. discussion 122. PMID: 10917354.
Article19. van Rooij WJ, Sluzewski M, Slob MJ, Rinkel GJ. Predictive value of angiographic testing for tolerance to therapeutic occlusion of the carotid artery. AJNR Am J Neuroradiol. 2005; 1. 26(1):175–178. PMID: 15661722.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Carotid-Cavernous Fistula Due to Giant Aneurysm in a Postpartum Woman
- Treatment of carotid-carvenous fistula and internal carotid aneurysm with Latex detachable balloons
- Regional Cerebral Blood Flow Changes in Traumatic Carotid Cavernous Fistula During Trapping Procedure: Case Study, Preliminary Report
- Treatment of Carotid-Cavernous Fistula and Internal Carotid Aneurysm with Debrun's Latex Detachable Balloon Catheter Technique
- Treatment of High-Flow Carotid Cavernous Fistula Using a Graft Stent: Case Report