Korean Circ J.
2016 Nov;46(6):879-881. 10.4070/kcj.2016.46.6.879.
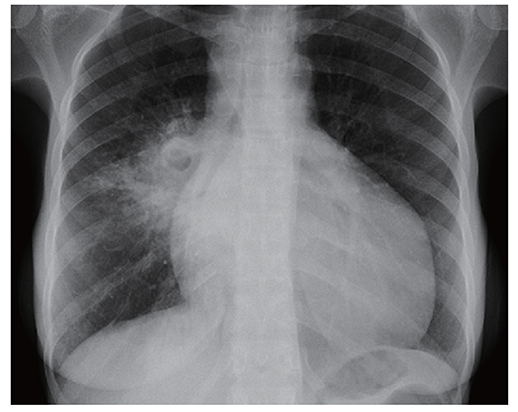
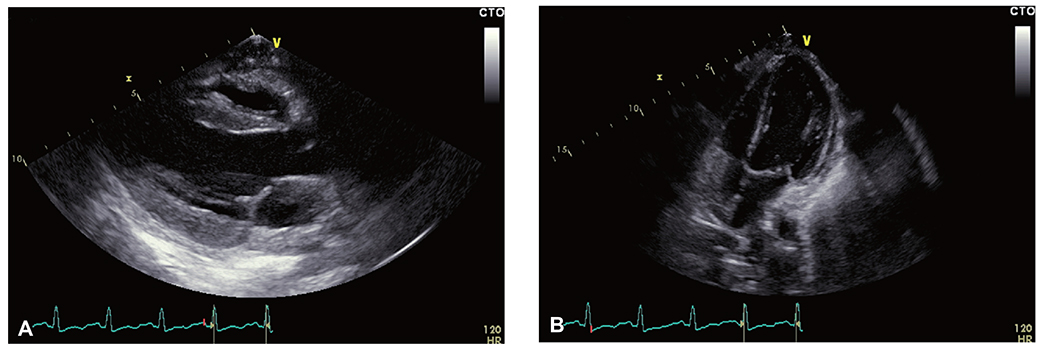
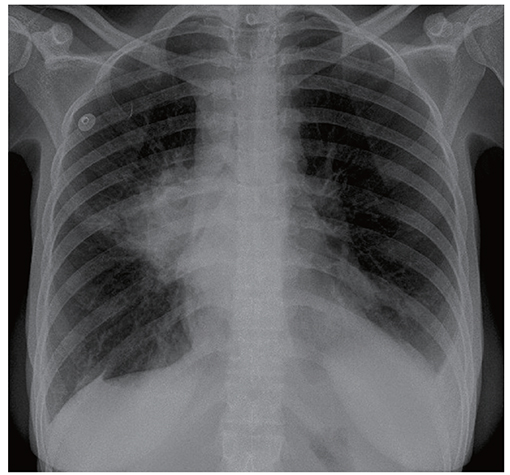
A "Vanishing", Tuberculous, Pericardial Effusion
- Affiliations
-
- 1Department of Internal Medicine, Kimberley Provincial Hospital, Du Toitspan Road, Kimberley Hospital, Kimberley, South Africa.
- 2SA Endovascular, Kuils River Hospital, Kuils River, South Africa. pieter.vanderbijl@gmail.com
- KMID: 2355468
- DOI: http://doi.org/10.4070/kcj.2016.46.6.879
Abstract
- We present an iatrogenic, pleuro-pericardial connection resulting from pericardiocentesis of a large, tuberculous, pericardial effusion. Recognition of this situation is paramount when one is unable to aspirate pericardial fluid after a successful, initial puncture. Such knowledge will help prevent myocardial or coronary artery injury with further attempts at aspiration.
MeSH Terms
Figure
Reference
-
1. Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004; 25:587–610.2. Tsang TS, Enriquez-Sarano M, Freeman WK, et al. Consecutive 1127 therapeutic echocardiographically guided pericardiocenteses: clinical profile, practice patterns and outcomes spanning 21 years. Mayo Clin Proc. 2002; 77:429–436.3. Badri M, Wilson D, Wood R. Effect of highly active antiretroviral therapy on incidence of tuberculosis in South Africa: a cohort study. Lancet. 2002; 359:2059–2064.4. Permanyer-Miralda G, Sagristá-Sauleda J, Soler-Soler J. Primary acute pericardial disease: a prospective series of 231 consecutive patients. Am J Cardiol. 1985; 56:623–630.5. Klein SV, Afridi H, Agarwal D, Coughlin BF, Schielke LH. CT directed diagnostic and therapeutic pericardiocentesis: 8-year experience at a single institution. Emerg Radiol. 2005; 11:353–363.6. Maggiolini S, Bozzano A, Russo P, et al. Echocardiography-guided pericardiocentesis with probe-mounted needle: report of 53 cases. J Am Soc Echocardiogr. 2001; 14:821–824.7. Tsang TS, Barnes ME, Hayes SN, et al. Clinical and echocardiographic characteristics of significant pericardial effusions following cardiothoracic surgery and outcomes of echo-guided pericardiocentesis for management: Mayo Clinic experience, 1979-1998. Chest. 1999; 116:322–331.8. Tsang TS, Freeman WK, Barnes ME, Reeder GS, Packer DL, Seward JB. Rescue echocardiographically guided pericardiocentesis for cardiac perforation complicating catheter-based procedures. The Mayo Clinic experience. J Am Coll Cardiol. 1998; 32:1345–1350.9. Winter M, Lim I, Joseph M. The disappearing pericardial effusion: a pericardial-pleural fistula. J Am Soc Echocardiogr. 2009; 22:973.e5–973.e7.10. Reuter H, Burgess L, van Vuuren W, Doubell A. Diagnosing tuberculous pericarditis. QJM. 2006; 99:827–839.11. Ziskind AA, Pearce AC, Lemmon CC, et al. Percutaneous balloon pericardiotomy for the treatment of cardiac tamponade and large pericardial effusions: description of technique and report of the first 50 cases. J Am Coll Cardiol. 1993; 21:1–5.12. El Haddad D, Iliescu C, Yusuf SW, et al. Outcomes of cancer patients undergoing percutaneous pericardiocentesis for pericardial effusion. J Am Coll Cardiol. 2015; 66:1119–1128.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT Findings of Tuberculous Pericardial Effusion
- The Usefulness of Pericardial Biopsy to Evaluate the Causes of Pericardial Disease
- Diagnostic Value of Adenosine Deaminase Activity in Tuberculous Pericardial Effusion
- A case of tuberculous pericarditis presenting as pericardial mass compressing pulmonary artery
- Two Cases of Primary HypoThyroidism Presenting with Pericardial Effusion