J Korean Fract Soc.
2016 Oct;29(4):270-275. 10.12671/jkfs.2016.29.4.270.
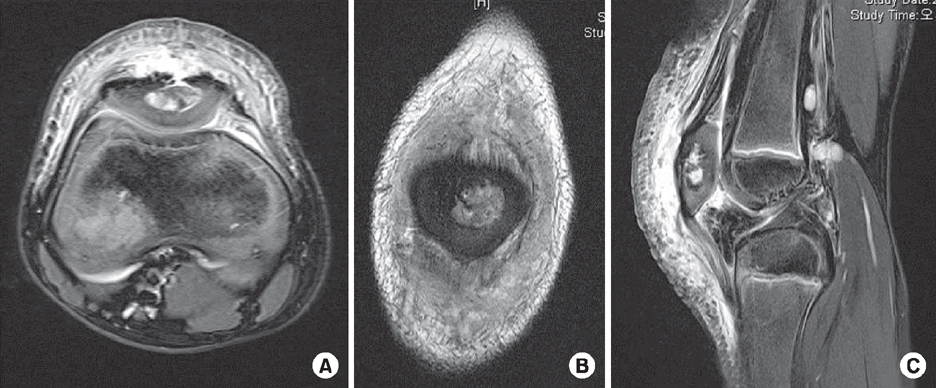
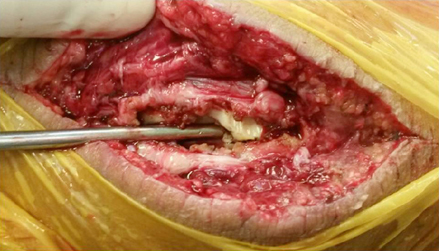
Acute Patellar Osteomyelitis in a Child after a Blunt Trauma: Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea. hjchung29@yonsei.ac.kr
- KMID: 2355433
- DOI: http://doi.org/10.12671/jkfs.2016.29.4.270
Abstract
- Osteomyelitis of the patella is a very uncommon condition that occurs mostly in the pediatric population. In addition to its rarity, nonspecific and variable clinical presentations usually lead to postponement in making the correct diagnosis. Moreover, it is often missed as prepatellar bursitis or septic arthritis of the knee. Nonetheless making early diagnosis and initiating prompt treatment is most important to preventing this condition from becoming chronic. In this case report, the authors encountered this rare condition of the patella in a child that was first misdiagnosed with pyogenic arthritis or prepatellar bursitis of the knee. The delay in making the diagnosis led to intractable progression of the disease, and sequestrectomy was required to stabilize the condition.
Keyword
MeSH Terms
Figure
Reference
-
1. Evans DK. Osteomyelitis of the patella. J Bone Joint Surg. 1962; 44:319–323.
Article2. de Gheldere A. Haematogenous osteomyelitis of the patella in a child. Acta Orthop Belg. 2009; 75:554–556.3. Kallfelz C, Wirbel R, Kriewitz M, Stölben A, von Laer L. Acute haematogenous osteomyelitis of the patella in childhood. Ann Orthop Rheumatol. 2015; 3:1046–1050.4. Durani Y, Attia MW. An unusual case of knee pain. Pediatr Emerg Care. 2006; 22:426–429.
Article5. Kankate RK, Selvan TP. Primary haematogenous osteomyelitis of the patella: a rare cause for anterior knee pain in an adult. Postgrad Med J. 2000; 76:707–709.
Article6. Choi HR. Patellar osteomyelitis presenting as prepatellar bursitis. Knee. 2007; 14:333–335.
Article7. Faust SN, Clark J, Pallett A, Clarke NM. Managing bone and joint infection in children. Arch Dis Child. 2012; 97:545–553.
Article8. Weichert S, Sharland M, Clarke NM, Faust SN. Acute haematogenous osteomyelitis in children: is there any evidence for how long we should treat? Curr Opin Infect Dis. 2008; 21:258–262.
Article9. Gil-Albarova J, Gómez-Palacio VE, Herrera A. Hematogenous osteomyelitis of the patella. J Pediatr Orthop B. 2012; 21:411–414.
Article10. Vaninbroukx J, Martens M, Verhelst M, Mulier JC. Haematogenous osteomyelitis of the patella. Report of three cases. Acta Orthop Scand. 1976; 47:566–569.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Osteomyelitis following Closed Femoral Shaft Fracture in a Child: A Case Report
- Osteomyelitis of the Patella in a Child: A Case Report
- Acute Extrapericardial Tamponade Caused by Blunt Chest Trauma: 2 case reports
- Acute Osteomyelitis in the Shaft of the Radius after Contusion of the Forearm: A Case Report
- Duodenal Injury after Blunt Abdominal Trauma: Report of Two Cases