J Korean Acad Psychiatr Ment Health Nurs.
2016 Sep;25(3):176-186. 10.12934/jkpmhn.2016.25.3.176.
Effects of an Education Program for Effective Nursing Intershift Handoff Communication on Nurses' Intershift Performance, Self-Efficacy, and Interrelationship Stress among Clinical Nurses: A Pilot Study
- Affiliations
-
- 1Department of Nursing, Kyung Dong University, Gosung, Korea.
- 2Department of German Language and Literature, Korea University, Seoul, Korea.
- 3Department of Korean Language and Literature, Gyeongin National University of Education, Incheon, Korea.
- 4Department of German Language and Literature, Korea University, Seoul, Korea.
- 5Department of Korean Language and Literature, Ewha Women University, Seoul, Korea.
- 6Graduate School of Education, Yonsei University, Seoul, Korea.
- 7College of Nursing Science, Kyung Hee University, Seoul, Korea. 5977sok@khu.ac.kr
- KMID: 2354864
- DOI: http://doi.org/10.12934/jkpmhn.2016.25.3.176
Abstract
- PURPOSE
The purpose of this study was to examine the effects of an education program for effective nursing intershift handoff communication (NIHC) on nursing intershift performance, self-efficacy, and interrelationship stress among clinical nurses.
METHODS
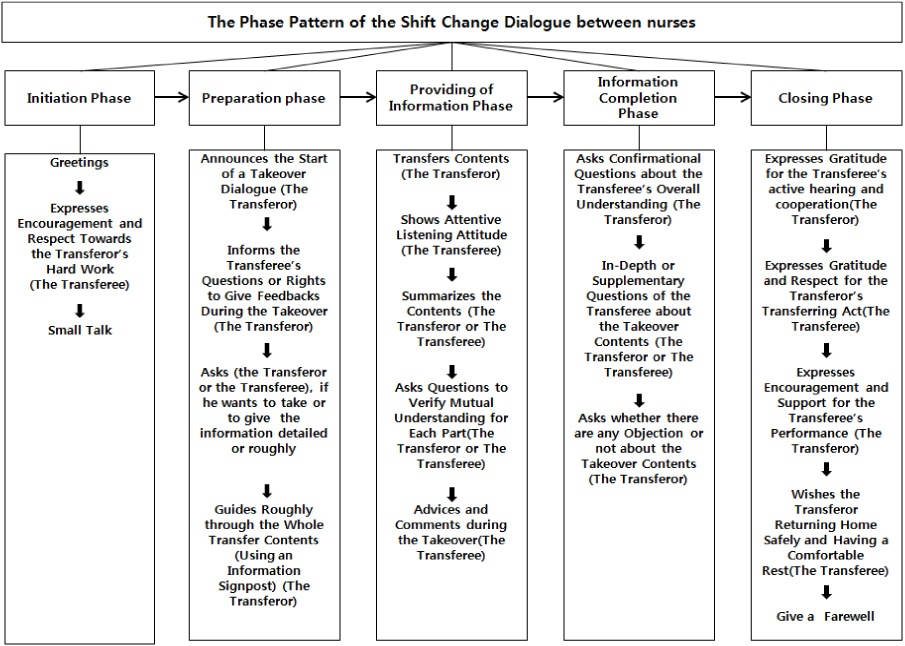
The study was a pilot study using a one-group pretest-posttest design. Participants were 40 clinical nurses from Seoul/ Gyeonggi Province. The handoff dialogue pattern was developed by three professors and one doctoral student in 2014, and was based on an education program for effective (NIHC) from dialogue analysis. The education program as an experimental treatment was provided for 3 1/2 hoursto clinical nurses. Measures included nursing intershift performance scale, self-efficacy scale, and interrelationship stress scale. Collected data was processed and analyzed with SPSS PC+ Version 21.
RESULTS
There were significant differences in nursing intershift performance (hand over: t=-12.18,p<.001; undertaking: t=-6.88, p<.001), self-efficacy (hand over: t=9.42, p<.001; undertaking: t=8.13, p<.001), and interrelationship stress (hand over: t=11.46, p<.001; undertaking: t=10.49, p<.001) between pre and post-test.
CONCLUSION
Findings indicate that this education program can be utilized as a manual, and can be applied to improve nursing intershift performance and self-efficacy, and to decrease interrelationship stress for effective (NIHC) among clinical nurses. Findings will also help to reduce incorrect performances and increase work efficiency in clinical practice for nurses.
Keyword
Figure
Reference
-
1. Benson E, Rippin-Sisler C, Jabusch K, Keast S. Improving nursing shift-to-shift report. J Nurs Care Qual. 2007; 22(1):80–84.
Article2. Jeoung YO, Bak YI. Communicative norms for the effective communication in nursing handover. J Textlinguistic Soc Korea. 2015; 38:121–143.3. Choi MH, Hong YS, Gem HA. Promotion of client's satisfaction through improvement of handoff method. In : Proceedings of Korean Society for Quality in Health Care Conference; 2005 November 24; Seoul, Korea. Seoul (Korea): Korean Society for Quality in Health Care;2005. p. 221–222. .4. Welsh CA, Flanagan ME, Ebright P. Barriers and facilitators to nursing handoffs: recommendations for redesign. Nurs Outlook. 2010; 58(3):148–154. DOI: 10.1016/j.outlook.2009.10.005.
Article5. Jeoung YO, Bak YI, Sok SH, Lee JW. Tool development to evaluate effective communication in nursing handover. Seoul Natl Univ J Hum. 2015; 72(2):507–542.
Article6. Lee HJ, Paik SB. A study on change-of-shift report as a nursing ritual. Res Sehan Univ. 2001; 7(1):377–386.7. Randella R, Wilson S, Woodward P. The importance of the verbal shift handover report: a multi-site case study. Int J Med Inform. 2011; 80(11):803–812. DOI: 10.1016/j.ijmedinf.2011.08.006.
Article8. Jeoung YO, Park SC, Jin JK, Kim JY, Lee JU, Park SY, et al. Content Analysis of Communication between Nurses during Preceptorship. J Korean Acad Psychiatr Ment Health Nurs. 2014; 23(2):82–92. DOI: 10.12934/jkpmhn.2014.23.2.82.
Article9. Hospital Nurses Association. Survey for effective handoff method development. Hospital Nurses Association Report. Seoul: HNA Press;2012. p. 3.10. Jeoung Y, Bak Y, Park S, Jin J, Baek SJ, Lee HY, et al. The handoff communication experience of nurses -focused on content analysis-. Korean J Health Commun. 2014; 9(1):61–71.11. Jeoung YO, Sok SH, Bak YI. The shift change dialogue pattern between nurses. Lang Linguist. 2015; 69:163–188.12. Faul F, Erdfelder E, Lang AG, Bunchner A. G*Power 3: a flexible statistical power analysis program for social, behavioral, and biochemical sciences. Behav Res Methods. 2007; 39:175–191.
Article13. Bak YI. Introdution into the dialog analysis. Seoul: Hyunmunsa;2014. p. 102.14. Kim AY, Cha JE. Self-efficacy and measurement. In : Korean Society for Industrial and Organizational Psychology Conference; 1996 Novemebr 30; Seoul, Korea. Seoul (Korea): Korean Society for Industrial and Organizational Psychology;1996. p. 16–22.15. Kim AY. Goal attainment theory and self-efficacy. In : Korean Society for Industrial and Organizational Psychology Conference; 1997 November 29; Seoul, Korea. Seoul (Korea): Korean Society for Industrial and Organizational Psychology;1997. p. 41–51.16. Cooper CL, Marshall J. Occupational sources of stress: a review of the literature relating to coronary heart disease and mental ill health. J Occup Psychol. 1976; 49(1):11–28. DOI: 10.1111/j.2044-8325.1976.tb00325.x.
Article17. Tak GG. The study on the effect of the stress due to interpersonal relations on job satisfaction [master's thesis]. Seoul: Hanyang University;2009. 78.18. Fenton W. Developing a guide to improve the quality of nurses' handover. Nurs Older People. 2006; 18(11):32–36.
Article19. Kim E, Kim S, Lee HY. Understanding perceptions of nursing hand over among Korean nurses. Korean Public Health Res. 2014; 40(4):41–49.20. Brown JA, Dunning CF, Cavanagh D, Cross LA. Enhancing midwives' scope of practice: an innovative educational program for delivery suite operating rooms. J Contin Educ Nurs. 2015; 46(2):89–96.
Article21. Delaney MM, Friedman MI, Dolansky MA, Fitzpatrick JJ. Impact of a sepsis educational program on nurse competence. J Contin Educ Nurs. 2015; 46(4):179–186. DOI: 10.3928/00220124-20150320-03.
Article22. Dowding D. Examining the effects that manipulating information given in the change of shift report has on nurses' care planning ability. J Adv Nurs. 2001; 33(6):836–846.
Article23. Hsu TC, Chiang-Hanisko L, Lee-Hsieh J, Lee GY, Turton MA, Tseng YJ. Effectiveness of an online caring curriculum in enhancing nurses' caring behavior. J Contin Educ Nurs. 2015; 46(9):416–424. DOI: 10.3928/00220124-20150821-04.
Article24. No YS, Kim SH, Yang SH, Kang YS. Clinical competence and self-confidence of new graduate nurses with an integrated nursing curriculum of simulation with problem-based learning. J Korea Academia-Industrial cooperation Soc. 2013; 14(7):3349–3357.
Article25. Park MW, Park EA. Effect of cultural competency education for nurse. Multicul Educ St. 2013; 6(2):115–133.26. Choi SJ. Development and evaluation of learning transfer based patient safety education program for new nurse [doctoral dissertation]. [Seoul]: Korea University;2014. 48.27. Kim YM, You MS, Cho YH, Park SH, Nam SN, Kim MY. Effects of a new-nurse education program utilizing E-learning and instructor demonstration on insulin injection practices. J Korean Cli Nurs Res. 2011; 7(3):411–420.28. Hsu LL, Huang YH, Hsieh SI. The effects of scenario-based communication training on nurses' communication competence and self-efficacy and myocardial infarction knowledge. Patient Educ Couns. 2014; 95(3):356–364. DOI: 10.1016/j.pec.2014.03.010.
Article29. Lin LM, Lin CC, Chen CL, Lin CC. Effects of an education program on intensive care unit nurses' attitudes and behavioral intentions to advocate deceased donor organ donation. Transplant Proc. 2014; 46(4):1036–1040. DOI: 10.1016/j.transproceed.2013.12.039.
Article30. Kim JH, Shin JS. Effects of an online problem-based learning program on sexual health care competencies among oncology nurses: a pilot study. J Contin Educ Nurs. 2014; 45(9):393–401.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of Handoff Education Program using SBAR for Nursing Students and Its Effect on Self-efficacy, Communication Ability and Clinical Performance Ability
- Assessment of Intershift Handoff in Emergency Medicine Training Hospitals in Korea
- Current domestic research trends on nurses’ communication programs
- Development and Feasibility of a Video Recording-Based Standardized Handoff Program for Ward Nurses: A pilot study
- Effects of Handoff Education using Concept Mapping and PASS-BAR