J Korean Soc Radiol.
2016 Oct;75(4):263-270. 10.3348/jksr.2016.75.4.263.
Endovascular Intervention as Management for Acute Limb Ischemia, Including the Rutherford Class IIb Ischemia: Korean Experience
- Affiliations
-
- 1Department of Radiology, CHA Bundang Medical Center, CHA University, Seongnam, Korea. hae0820@naver.com
- 2Department of Radiology and Medical Research Institute, Ewha Womans University Mokdong Hospital, Seoul, Korea.
- 3Department of Radiology, Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Thoracic & Cardiovascular Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- KMID: 2353676
- DOI: http://doi.org/10.3348/jksr.2016.75.4.263
Abstract
- PURPOSE
To comparatively assess the outcomes between endovascular intervention and surgery as initial management for acute limb ischemia (ALI).
MATERIALS AND METHODS
From April 2004 to March 2015, the medical records of 51 patients with ALI who were treated with intervention or surgery were reviewed. Patient baseline characteristics and procedural data were collected. Clinical outcomes were compared between patients classified according to the Rutherford criteria.
RESULTS
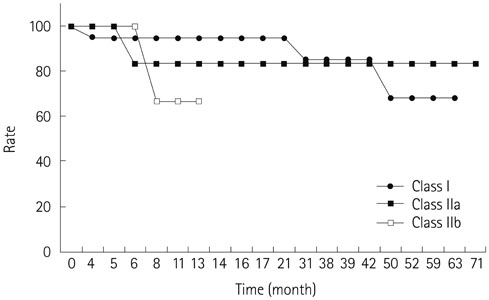
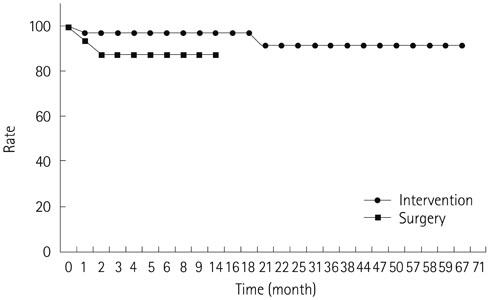
A total of 39 limbs of 35 patients underwent intervention, and 16 limbs of 16 patients underwent surgery. The technical success rate was 82.1% and 75.0% in the intervention and surgery groups, respectively. The intervention group showed no procedure related mortality or major complication during follow-up, but one case of compartment syndrome was reported in the surgery group. The mean follow-up period was 23.4 and 16.6 months in the intervention and surgery groups, respectively. The primary patency rate at 12 months was 89.4% and 100%, and the limb salvage rate at 12 months was 97.2% and 87.1% in the intervention and surgery groups, respectively. Among 7 patients with technical failure of intervention, immediate surgery was required in 6 cases, and 2 major and 1 minor amputations were required during follow-up.
CONCLUSION
Endovascular therapy is a safe and effective treatment option that reduces and delays amputation in patients with ALI.
MeSH Terms
Figure
Cited by 1 articles
-
Effectiveness of Percutaneous Aspiration Thrombectomy for Acute or Subacute Thromboembolism in Infrainguinal Arteries
Jung Guen Cha, Chan Sun Kim, Young Hwan Kim, See Hyung Kim
J Korean Soc Radiol. 2017;76(6):386-394. doi: 10.3348/jksr.2017.76.6.386.
Reference
-
1. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. TASC II Working Group. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007; 45:Suppl S. S5–S67.2. Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997; 26:517–538.3. Results of a prospective randomized trial evaluating surgery versus thrombolysis for ischemia of the lower extremity. The STILE trial. Ann Surg. 1994; 220:251–266. discussion 266-268.4. Ouriel K, Veith FJ, Sasahara AA. A comparison of recombinant urokinase with vascular surgery as initial treatment for acute arterial occlusion of the legs. Thrombolysis or Peripheral Arterial Surgery (TOPAS) Investigators. N Engl J Med. 1998; 338:1105–1111.5. Rutherford RB. Clinical staging of acute limb ischemia as the basis for choice of revascularization method: when and how to intervene. Semin Vasc Surg. 2009; 22:5–9.6. Løkse Nilssen GA, Svendsen D, Singh K, Nordhus K, Sørlie D. Results of catheter-directed endovascular thrombolytic treatment of acute ischaemia of the leg. Eur J Vasc Endovasc Surg. 2011; 41:91–96.7. Kashyap VS, Gilani R, Bena JF, Bannazadeh M, Sarac TP. Endovascular therapy for acute limb ischemia. J Vasc Surg. 2011; 53:340–346.8. Rajan DK, Patel NH, Valji K, Cardella JF, Bakal C, Brown D, et al. Quality improvement guidelines for percutaneous management of acute limb ischemia. J Vasc Interv Radiol. 2005; 16:585–595.9. Ansel GM, Botti CF Jr, Silver MJ. Treatment of acute limb ischemia with a percutaneous mechanical thrombectomy-based endovascular approach: 5-year limb salvage and survival results from a single center series. Catheter Cardiovasc Interv. 2008; 72:325–330.10. Oğuzkurt L, Ozkan U, Gümüs¸ B, Coükun I, Koca N, Gülcan O. Percutaneous aspiration thrombectomy in the treatment of lower extremity thromboembolic occlusions. Diagn Interv Radiol. 2010; 16:79–83.11. McNamara T, Goodwin S, Kandarpa K. Complications of thrombolysis. Semin Interv Radiol. 1994; 11:134–144.12. Ouriel K, Welch EL, Shortell CK, Geary K, Fiore WM, Cimino C. Comparison of streptokinase, urokinase, and recombinant tissue plasminogen activator in an in vitro model of venous thrombolysis. J Vasc Surg. 1995; 22:593–597.13. Lyden SP. Endovascular treatment of acute limb ischemia: review of current plasminogen activators and mechanical thrombectomy devices. Perspect Vasc Surg Endovasc Ther. 2010; 22:219–222.14. Kim YH, Bae JI, Jeon YS, Kim CW, Jae HJ, Park KB, et al. Guideline for interventional recanalization of lower extremity artery. J Korean Soc Radiol. 2014; 71:205–230.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catheter-Directed Thrombolysis for Persistent Sciatic Artery Presenting with Acute Limb Ischemia
- Endovascular treatment of acute limb ischemia due to thrombotic occlusion of the suprainguinal artery
- Clinical Comprehension and Application of Angiosome Concept in Critical Limb Ischemia
- Acute Myeloid Leukemia with Intracardiac Thrombus Presenting as Acute Limb Ischemia
- Endovascular Strategies in the Management of Acute Limb Ischemia