J Korean Ophthalmol Soc.
2016 Sep;57(9):1435-1440. 10.3341/jkos.2016.57.9.1435.
The Clinical Features and the Prognosis of Functional Visual Loss in Children
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University School of Medicine, Daejeon, Korea. opticalyh@hanmail.net
- 2Research Institute for Medical Sciences, Chungnam National University, Daejeon, Korea.
- KMID: 2351875
- DOI: http://doi.org/10.3341/jkos.2016.57.9.1435
Abstract
- PURPOSE
To evaluate the clinical characteristics and prognoses of children with functional visual loss.
METHODS
Retrospective medical record review was performed in 53 patients 4 to 16 years of age diagnosed with functional visual loss between April 2006 and February 2014. We investigated the clinical features and results of clinical tests and the final status of the patients.
RESULTS
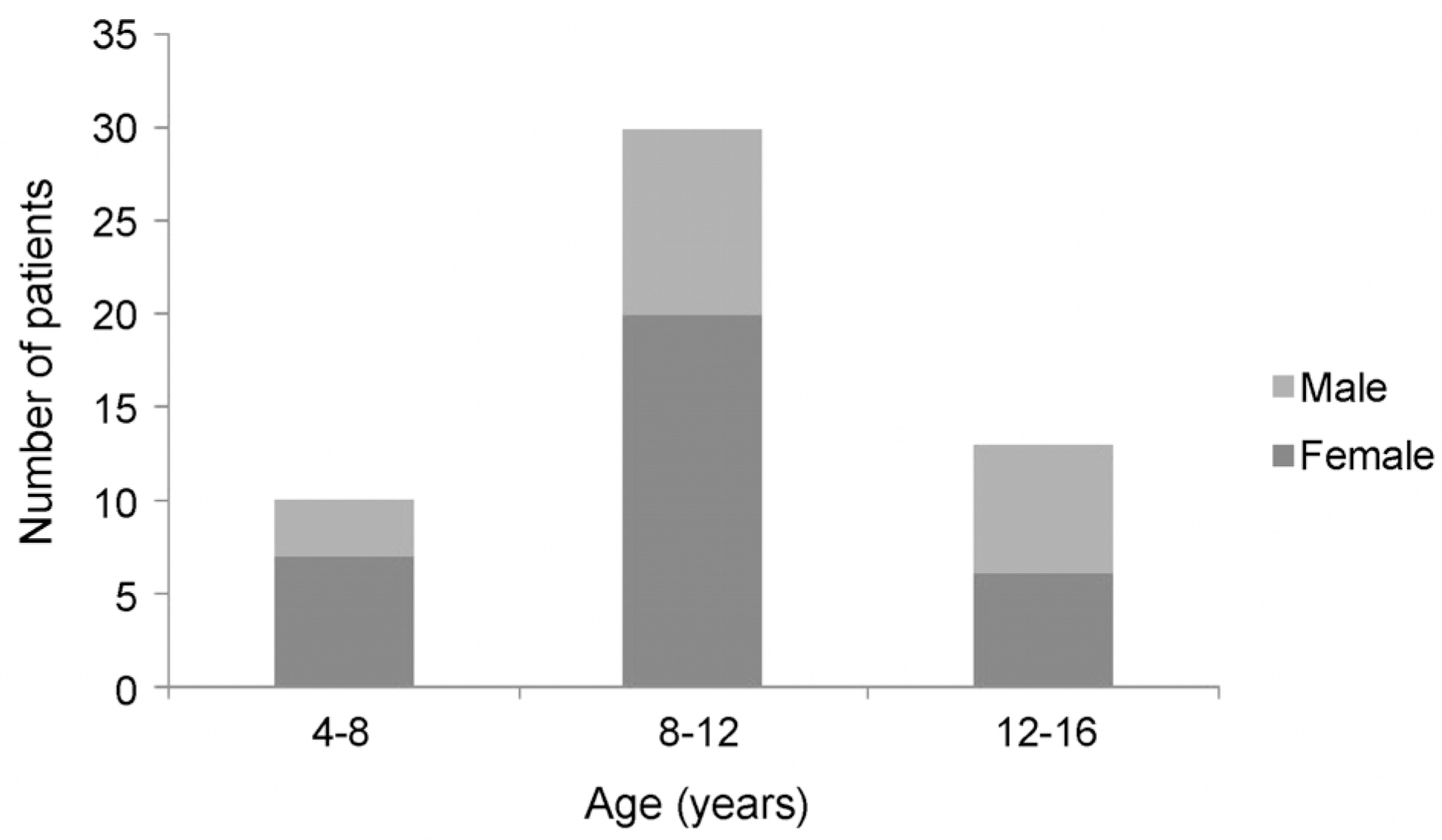
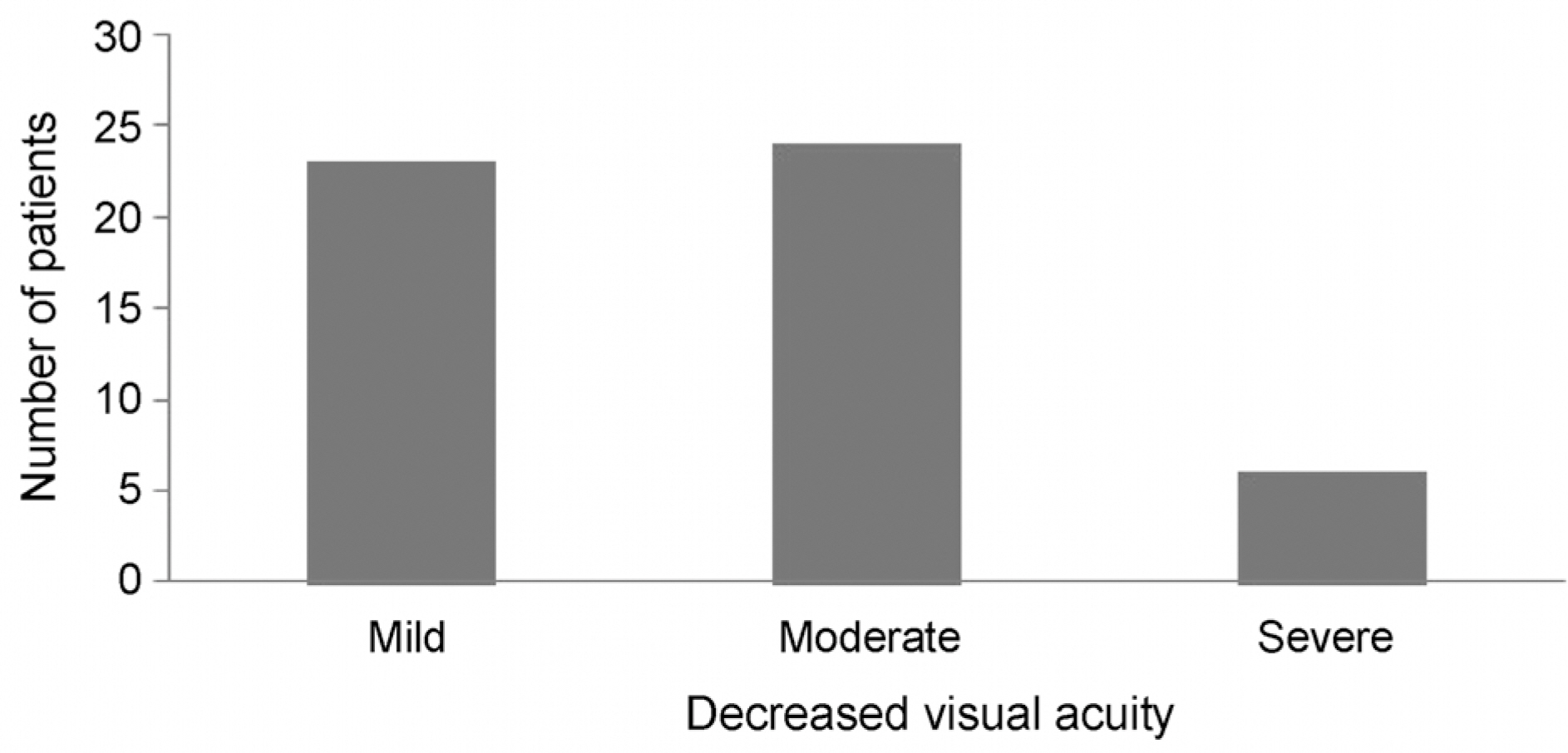
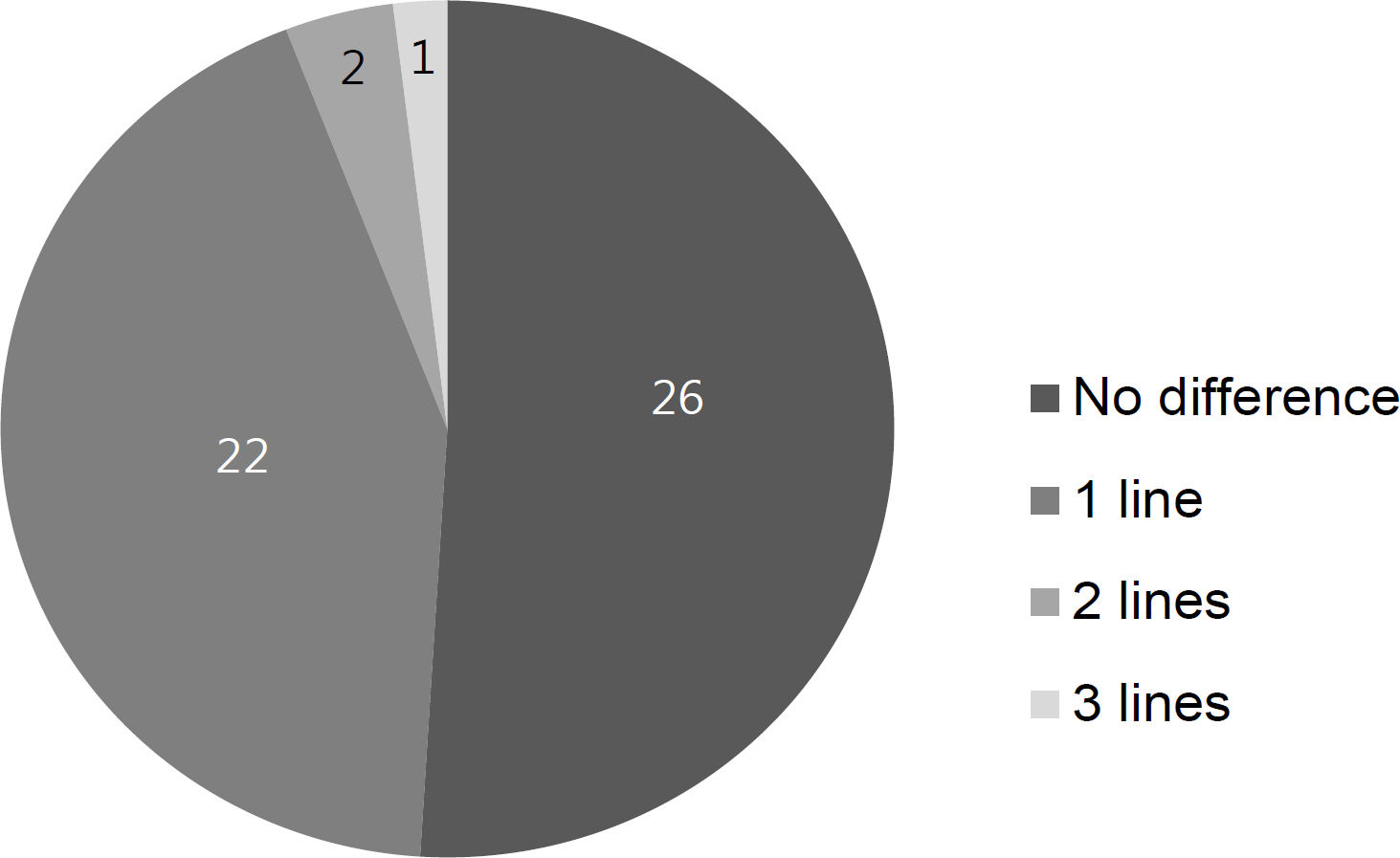
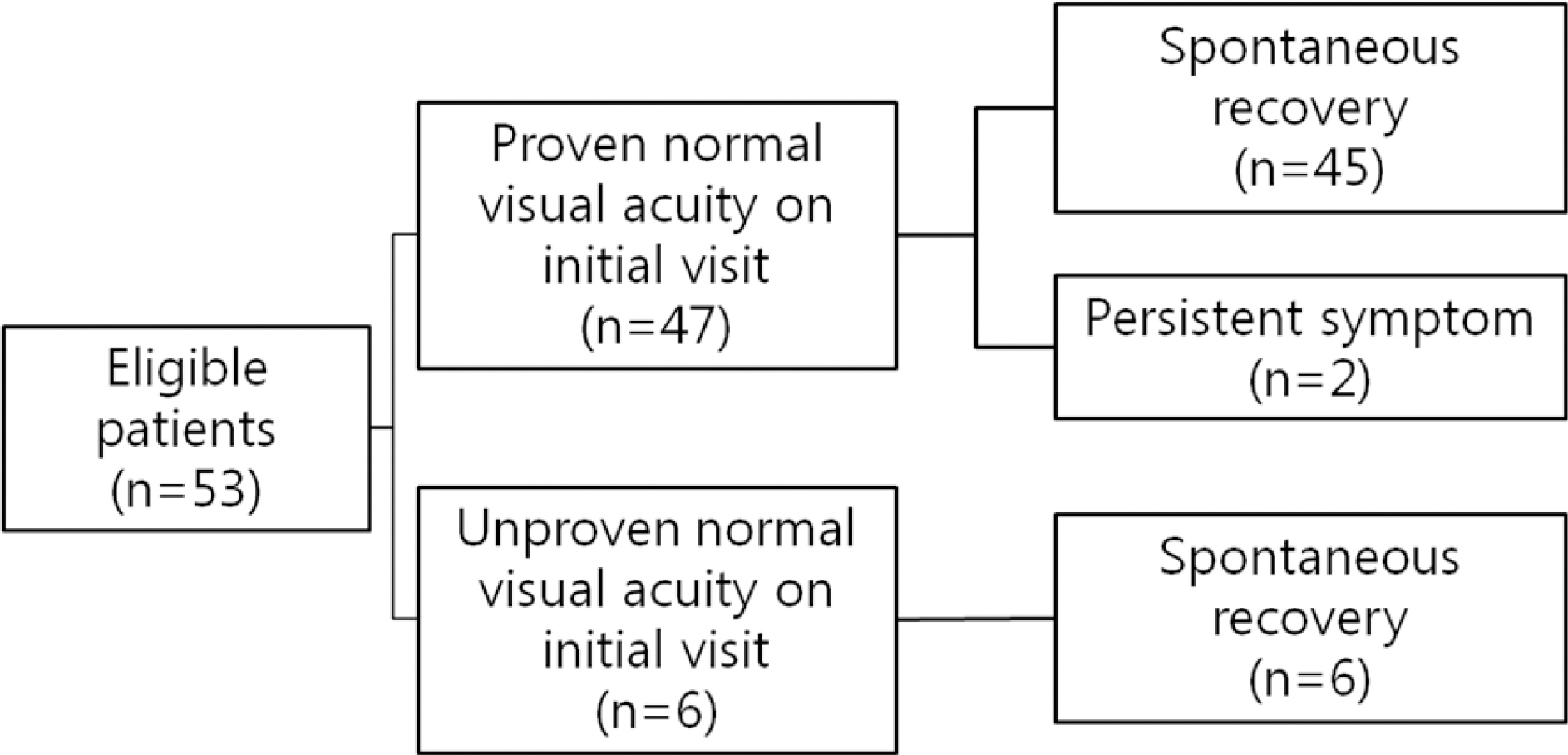
Twenty male (37.8%) and 33 female (62.2%) patients were included in the study. The mean age was 9.69 ± 2.76 years. The incidence was highest between 8 to 12 years. The mean best corrected visual acuity at baseline was 0.43 ± 0.23, and 88.7% of patients had mild to moderate visual loss. The symptoms were bilateral in 96.2% of patients, and the difference of corrected visual acuity between two eyes was 1 line or less on Snellen chart in 94.1% of bilateral cases. The symptoms were resolved by 1.8 ± 1.0 months in 59.5% of patients and resolved by the final follow-up visit in 51 (96.2%). However, the symptoms persisted through the final follow-up in 2 patients.
CONCLUSIONS
Most children with functional visual loss have bilateral and mild to moderate visual loss. The prognosis of functional visual loss in children was excellent. Most patients recovered from the disease with reassurance supportive care without psychiatric treatment, although a few patients had persistent symptoms.
MeSH Terms
Figure
Reference
-
References
1. Kathol RG, Cox TA, Corbett JJ, Thompson HS. Functional visual loss. Follow-up of 42 cases. Arch Ophthalmol. 1983; 101:729–35.2. Miller NR, Newman NJ, Biousse V, Kerrison JB. Walsh and Hoyt's Clinical Neuro-Ophthalmology. 6th ed.1. Baltimore: Williams & Wilkins;2005. p. 1315–34.3. Ney JJ, Volpe NJ, Liu GT, et al. Functional visual loss in idiopathic intracranial hypertension. Ophthalmology. 2009; 116:1808–13.e1.
Article4. Egan RA. Functional visual loss. Ophthalmol Clin North Am. 2004; 17:321–8. vi.
Article5. Bose S, Kupersmith MJ. Neuro-ophthalmologic presentations of functional visual disorders. Neurol Clin. 1995; 13:321–39.
Article6. Catalano RA, Simon JW, Krohel GB, Rosenberg PN. Functional visual loss in children. Ophthalmology. 1986; 93:385–90.
Article7. Taich A, Crowe S, Kosmorsky GS, Traboulsi EI. Prevalence of psychosocial disturbances in children with nonorganic visual loss. J AAPOS. 2004; 8:457–61.
Article8. Clarke WN, Noël LP, Bariciak M. Functional visual loss in children: a common problem with an easy solution. Can J Ophthalmol. 1996; 31:311–3.9. Mäntyjärvi MI. The amblyopic schoolgirl syndrome. J Pediatr Ophthalmol Strabismus. 1981; 18:30–3.
Article10. van Balen AT, Slijper FE. Psychogenic amblyopia in children. J Pediatr Ophthalmol Strabismus. 1978; 15:164–7.
Article11. Toldo I, Pinello L, Suppiej A, et al. Nonorganic (psychogenic) abdominal loss in children: a retrospective series. J Neuroophthalmol. 2010; 30:26–30.12. Lee SM, Lim MH, Kyung SE. Child behavior check list, Korean personality inventory for children in presumed functional visual loss. J Korean Ophthalmol Soc. 2010; 51:1092–8.
Article13. Kang YH, Yu YS. Functional visual loss in children. J Korean Ophthalmol Soc. 1996; 37:2118–24.14. Kim JS, Hwang JM. Clinical Neuro-Ophthalmology. 1st ed.Seoul: E-public;2010. p. 288–303.15. Miller BW. A review of practical tests for ocular malingering and hysteria. Surv Ophthalmol. 1974; 17:241–6.16. Sletteberg O, Bertelsen T, Høvding G. The prognosis of patients with hysterical visual impairment. Acta Ophthalmol (Copenh). 1989; 67:159–63.
Article17. Hafeiz HB. Hysterical conversion: a prognostic study. Br J Psychiatry. 1980; 136:548–51.
Article18. Yasuna ER. Hysterical amblyopia in children. Am J Dis Child. 1963; 106:558–63.
Article19. Krill AE, Newell FW. The diagnosis of ocular conversion reaction involving visual function. Arch Ophthalmol. 1968; 79:254–61.
Article20. Rada RT, Meyer GG, Krill AE. Visual conversion reaction in children. I. Diagnosis. Psychosomatics. 1969; 10:23–8.
Article21. Bain KE, Beatty S, Lloyd C. Non-organic visual loss in children. Eye (Lond). 2000; 14(Pt 5):770–2.
Article22. Barris MC, Kaufman DI, Barberio D. Visual impairment in hysteria. Doc Ophthalmol. 1992; 82:369–82.
Article23. Kramer KK, La Piana FG, Appleton B. Ocular malingering and hysteria: diagnosis and management. Surv Ophthalmol. 1979; 24:89–96.
Article24. Keltner JL, May WN, Johnson CA, Post RB. The California syndrome. Functional visual complaints with potential economic impact. Ophthalmology. 1985; 92:427–35.25. Lim SA, Siatkowski RM, Farris BK. Functional visual loss in adults and children patient characteristics, management, and outcomes. Ophthalmology. 2005; 112:1821–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Child Behavior Check List, Korean Personality Inventory for Children in Presumed Functional Visual Loss
- Functional Visual Loss in Children
- The Effectiveness of Visual Evoked Potentials in Disability Evaluation
- Treatment and Prognosis of Cataract in Children
- An Analysis of Visual Fields in Patients with Post-traumatic Functional Visual Loss