J Korean Ophthalmol Soc.
2016 Sep;57(9):1354-1360. 10.3341/jkos.2016.57.9.1354.
Reliability of a New Non-invasive Tear Film Break-up Time Measurement Using a Keratograph
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. sbummlee@ynu.ac.kr
- KMID: 2351864
- DOI: http://doi.org/10.3341/jkos.2016.57.9.1354
Abstract
- PURPOSE
To evaluate the repeatability of non-invasive tear film break-up time and identify its relationships with dry eye parameters.
METHODS
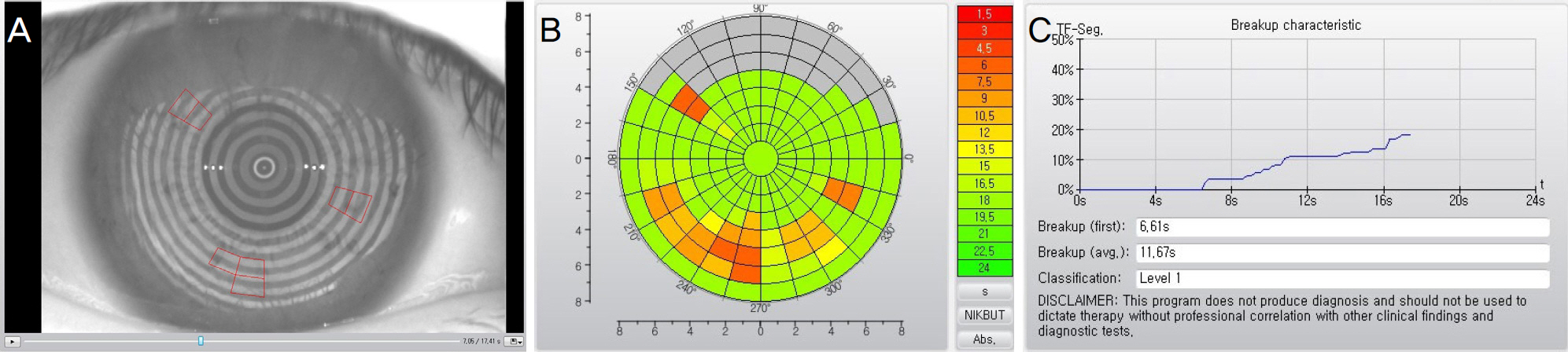
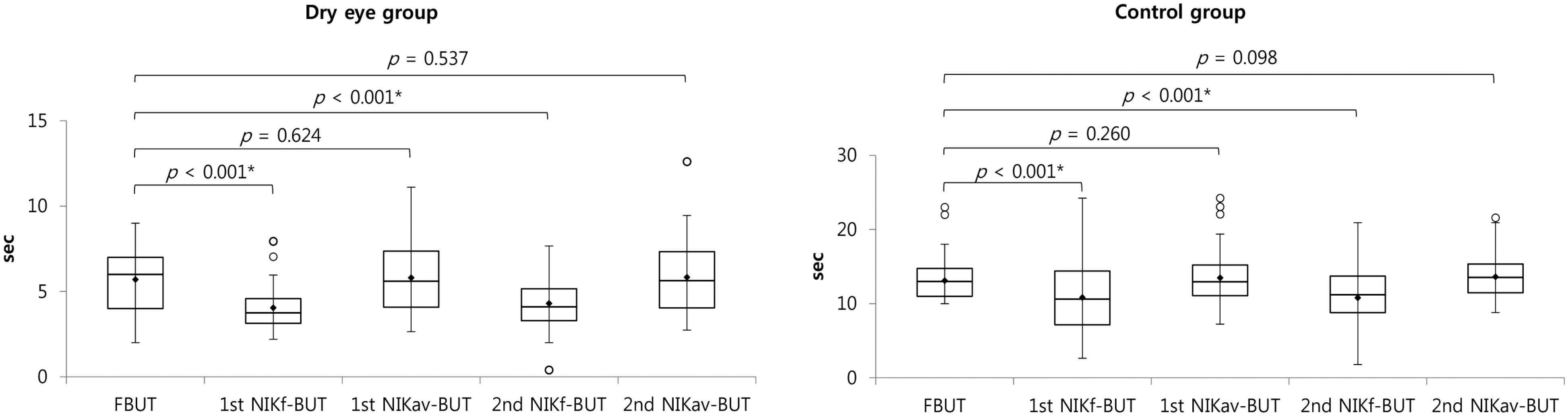
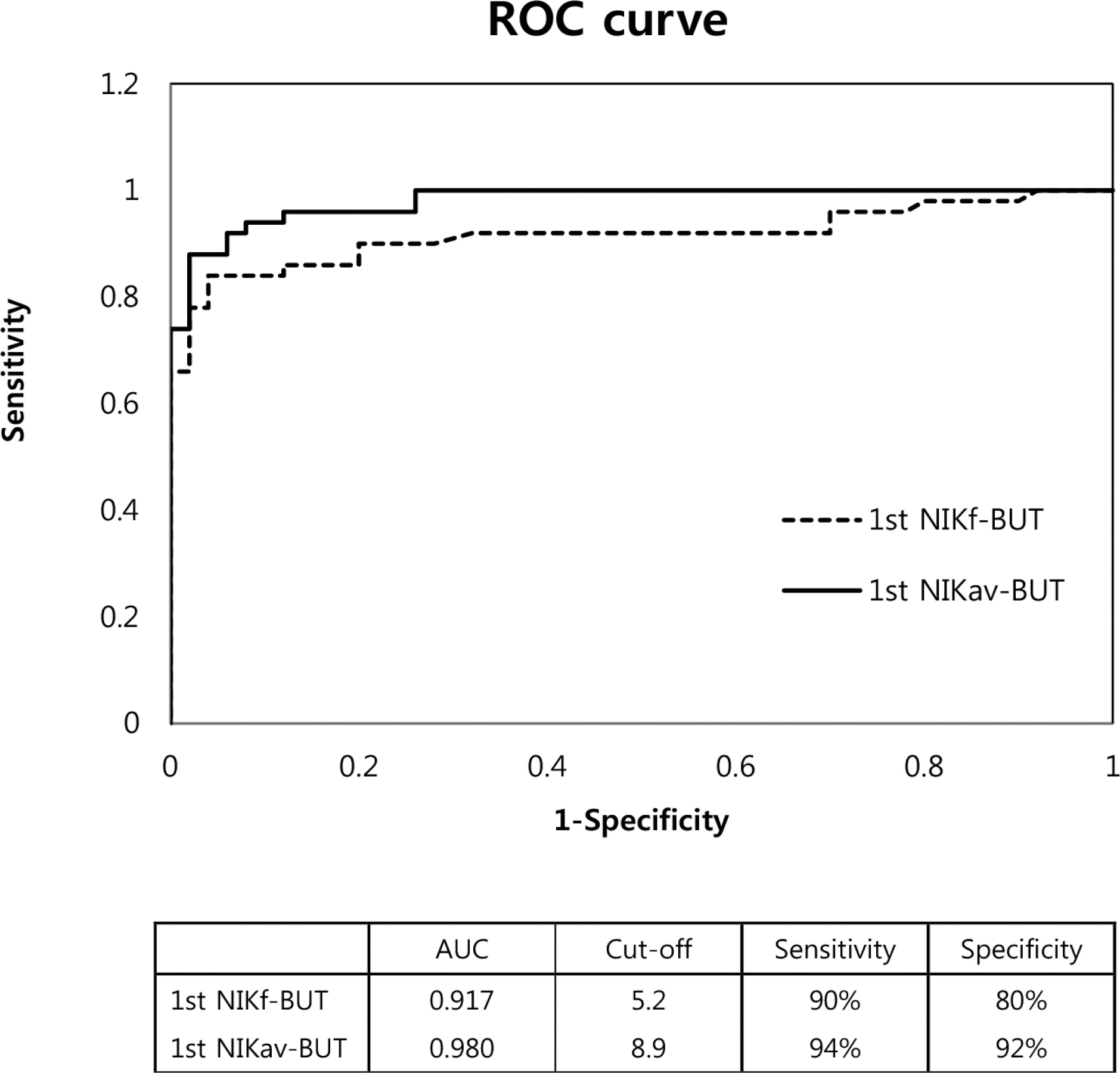
A total of 100 participants (50 with dry eye, and 50 in the control group) were enrolled prospectively. Non-invasive keratograph first (NIKf-BUT) and average (NIKav-BUT) break-up times were evaluated 2 times using Keratograph 4 (Oculus, Wetzler, Germany), and then tear film break-up time with fluorescein (FBUT) was measured. The correlation analyses were performed between non-invasive parameters (NIKf-BUT and NIKav-BUT) and FBUT. Intra-observer agreements of NIKf-BUT and NIKav-BUT were assessed using intraclass correlation coefficients (ICC). The receiver operating characteristic (ROC) curve technique was used to evaluate the non-invasive method in the diagnosis of dry eye.
RESULTS
The correlation analyses revealed positive correlation between NIKav-BUT and FBUT in both groups (dry eye; r = 0.66, p < 0.001 and control group; r = 0.77, p < 0.001). The ICCs of NIKf-BUT and NIKav-BUT were 0.72 and 0.94 in the dry eye, respectively, and 0.70 and 0.91 in the control group. NIKav-BUT was not different from FBUT in either group. The areas under the ROC curves of NIKf-BUT and NIKav-BUT were 0.917 and 0.980, respectively.
CONCLUSIONS
The high ICCs verified the repeatability of NIKf-BUT and NIKav-BUT. NIKav-BUT showed no difference from FBUT and positive correlation with FBUT. NIK-BUT showed high diagnostic power and can be considered a new parameter to evaluate dry eye syndrome.
MeSH Terms
Figure
Cited by 1 articles
-
The Use of Keratography to Study Changes on the Ocular Surface after Absorbable Plug Insertion
Hee Jong Shin, Chang-Hyun Park, Kyung Sun Na, Hyun Seung Kim
J Korean Ophthalmol Soc. 2018;59(1):17-22. doi: 10.3341/jkos.2018.59.1.17.
Reference
-
References
1. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.2. Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the abdominal and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol. 2014; 28:197–206.3. Norn MS. Desiccation of the precorneal film. I. Corneal wet-ting-time. Acta Ophthalmol (Copenh). 1969; 47:865–80.4. Mengher LS, Bron AJ, Tonge SR, Gilbert DJ. Effect of fluorescein instillation on the precorneal tear film stability. Curr Eye Res. 1985; 4:9–12.
Article5. Patel S, Murray D, McKenzie A, et al. Effects of fluorescein on tear breakup time and on tear thinning time. Am J Optom Physiol Opt. 1985; 62:188–90.
Article6. Mengher LS, Bron AJ, Tonge SR, Gilbert DJ. A non-invasive instrument for clinical assessment of the precorneal tear film stability. Curr Eye Res. 1985; 4:1–7.
Article7. Cox SM, Nichols KK, Nichols JJ. Agreement between automated and traditional measures of tear film breakup. Optom Vis Sci. 2015; 92:e257–63.
Article8. Hong J, Sun X, Wei A, et al. Assessment of tear film stability in dry eye with a newly developed keratograph. Cornea. 2013; 32:716–21.
Article9. Jiang Y, Ye H, Xu J, Lu Y. Noninvasive Keratograph assessment of tear film break-up time and location in patients with age-related cataracts and dry eye syndrome. J Int Med Res. 2014; 42:494–502.
Article10. Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000; 118:615–21.
Article11. Korb DR. Survey of preferred tests for diagnosis of the tear film and dry eye. Cornea. 2000; 19:483–6.
Article12. Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea. 2004; 23:272–85.
Article13. Lee JH, Kee CW. The significance of tear film break-up time in the diagnosis of dry eye syndrome. Korean J Ophthalmol. 1988; 2:69–71.
Article14. Goto E, Tseng SC. Differentiation of lipid tear deficiency dry eye by kinetic analysis of tear interference images. Arch Ophthalmol. 2003; 121:173–80.
Article15. Guillon JP. Use of the Tearscope Plus and attachments in the abdominal examination of the marginal dry eye contact lens patient. Adv Exp Med Biol. 1998; 438:859–67.16. Best N, Drury L, Wolffsohn JS. Clinical evaluation of the Oculus Keratograph. Cont Lens Anterior Eye. 2012; 35:171–4.
Article17. Cho P, Douthwaite W. The relation between invasive and non-invasive tear break-up time. Optom Vis Sci. 1995; 72:17–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Loose Masks on Tear-film Break-up Time
- A Comparison between Keratograph 5M® and IDRA® in Dry Eye Patients
- A Pilot Study of Changes in Tear Film Short-term Dynamics with Infrared Imaging after Phacoemulsification
- Comparison of Each Eye According to the Order of Noninvasive Keratographic Tear Film Evaluation
- Effects of Non-invasive Keratograph Break-Up Time on the Repeatability of Keratometry Measurements