Korean J Adult Nurs.
2014 Feb;26(1):98-106. 10.7475/kjan.2014.26.1.98.
The Effect of Glove Changing during Surgery for Colon Cancer
- Affiliations
-
- 1Konkuk University Hospital Operating Room, Seoul, Korea.
- 2Department of Nursing, Konkuk University, Chungju, Korea. Hem2003@kku.ac.kr
- KMID: 2351594
- DOI: http://doi.org/10.7475/kjan.2014.26.1.98
Abstract
- PURPOSE
The purpose of this study was to explore the effect of glove changing during surgery for colon cancer on reducing the degree of contamination of surgical gloves.
METHODS
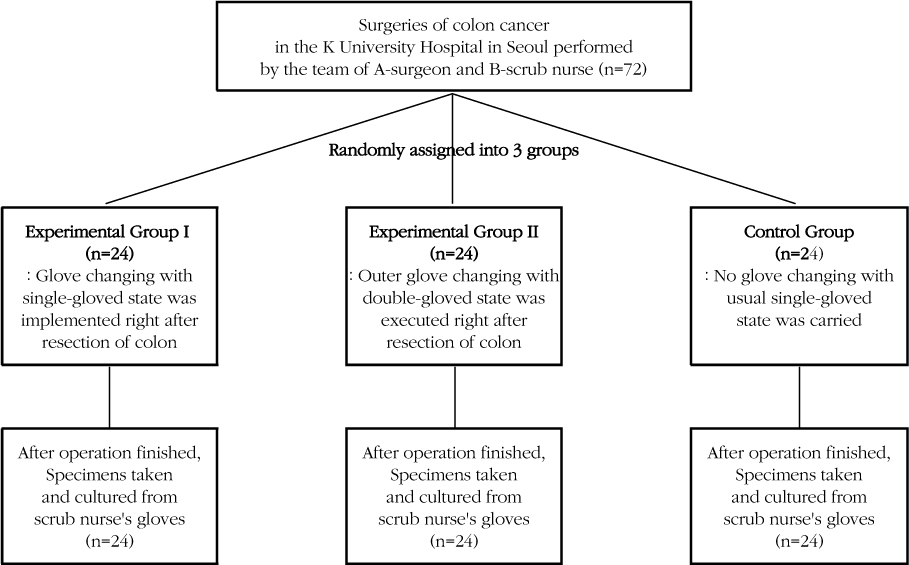
The randomized posttest control group design was used. Total 72 surgeries of colon cancer in the K University Hospital in Seoul performed by the team of A-Surgeon and B-Scrub nurse were randomly assigned to one of the three groups. Glove changing with single-gloved state was implemented in the Experimental Group I and outer glove changing with double-gloved state was executed in the Experimental Group II. Single-gloved state was carried in the Control Group. Following the surgical procedure, specimens for bacterial culture were collected the from scrub nurse's gloves to compare the degree of contamination among the three groups. Data were analyzed with One-way ANOVA and the Scheffe's multiple comparison test.
RESULTS
The degrees of contamination of the Experimental Group I and II were significantly lower than that of the Control Group. There was no significant difference between Experimental Group I and II.
CONCLUSION
Glove changing during surgery with either single or double-gloved state is effective in reducing the degree of contamination of surgical gloves, therefore these methods should be utilized in clinical practice.
Figure
Reference
-
1. Al-Maiyah M, Bajwa A, Finn P, Mackenney P, Hill D, Port A. Glove perforation and contamination in primary total hip arthroplasty. J Bone Joint Surg Br. 2005; 87(4):556–559. DOI: 10.1302/0301-620X.87B4.15744.
Article2. ASTM, West Conshohocken. ASTM D3577-09e1: Standard specification for rubber surgical gloves. 2009. 02. Retrieved January 10, 2011. from ASTM International Web site: http://www.astm.org/Standards/D3577.htm.3. Beldame J, Lagrave B, Lievain L, Lefebvre B, Frebourg N, Dujardin F. Surgical glove bacterial contamination and perforation during total hip arthroplasty implantation: When gloves should be changed. Orthopaedics Traumatology: Surgery Resear. Orthop Traumatol Surg Res. 2012; 98(4):432–440. DOI: 10.1016/j.otsr.2011.10.015.4. Chapin DW. Surgical gloves: Make the right choice. OR Nurse. 2007; 1(6):13–14.5. Cho OY, Yoon HS. Effect of the exchange of saline used in surgical procedures on surgical site infection. J Korean Acad Nurs. 2004; 34(3):467–476.
Article6. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed.New Jersey: Lawrence Erlbaum Associates;1988.7. Daeschlein G, Kramer A, Arnold A, Ladwig A, Seabrook GR, Edmiston CE Jr. Evaluation of an innovative antimicrobial surgical glove technology to reduce the risk of microbial passage following intraoperative perforation. Am J Infect Control. 2011; 39(2):98–103. DOI: 10.1016/j.ajic.2010.05.026.
Article8. Daniels R, Nicoll LH. Contemporary medical-Surgical nursing. 8th ed. Philadelphia: W. B. Saunders;2011.9. Dawson-Bowling S, Smith J, Butt D, Cottam H, Umasankar S, Armitage A. Should outer surgical gloves be changed intraoperatively before orthopaedic prosthesis implantation? J Hosp Infect. 2011; 78(2):156–157. DOI: 10.1016/j.jhin.2011.02.014.
Article10. Ellis H. Surgical gloves. J Perioper Pract. 2010; 29(6):219–220.
Article11. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39(2):175–191.12. Guo YP, Wong PM, Li Y, Or PP. Is double-gloving really protective? A comparison between the glove perforation rate among perioperative nurses with single and double gloves during surgery. Am J Surg. 2012; 204(2):210–215. DOI: 10.1016/j.amjsurg.2011.08.017.
Article13. Harnoss JC, Parteck LI, Heidecke CD, Jubner NO, Kramer A, Assadian O. Concentration of bacteria passing through puncture holes in surgical gloves. Am J Infect Control. 2010; 38(2):154–158. DOI: 10.1016/j.ajic.2009.06.013.14. Hübner NO, Goerdt AM, Stanislawski N, Assadian O, Heldecke CD, Kramer A, et al. Bacterial migration through punctured surgical gloves under real surgical conditions. BMC Infect Dis. 2010; 1(10):192. DOI: 10.1186/1471-2334-10-192.
Article15. Kaya I, Ugras A, Sungur I, Yilmaz M, Korkmaz M, Cetinus E. Glove perforation time and frequency in total hip arthroplasty procedures. Acta Orthop Traumatol Turc. 2012; 46(1):57–60. DOI: 10.3944/AOTT.2012.2660.
Article16. Kim EJ, Koh MS. Character analysis that influences to surgical gloves punctures. J Korean Clin Nurs Res. 2012; 18(1):99–110.17. Kim JB, Lee HY, Kim YK, Ryu JG, Eom YB, Lee DS, et al. Pathogenic microbiology. Seoul: Life Science;2012.18. Lancaster C, Duff P. Single versus double-gloving for obstetric and gynecologic procedures. Am J Obstet Gynecol. 2007; 196(5):e36–e37. DOI: 10.1016/j.ajog.2006.08.045.
Article19. McCue SF, Berg EW, Saunders EA. Efficacy of double-gloving as a barrier to microbial contamination during total joint arthroplasty. J Bone Joint Surg Am. 1981; 63(5):811–813.
Article20. Misteli H, Weber WP, Reck S, Rosenthal R, Zwahlen M, Fueglistaler P, et al. Surgical glove perforation and the risk of surgical site infection. Arch Surg. 2009; 144(6):553–558. DOI: 10.1001/archsurg.2009.60.
Article21. Punyatanasakchai P, Chittacharoen A, Ayudhya NI. Randomized controlled trial of glove perforation in single- and double-gloving in episiotomy repair after vaginal delivery. J Obstet Gynaecol Res. 2004; 30(5):354–357. DOI: 10.1111/j.1447-0756.2004.00208.x.
Article22. Thomas S, Agarwal M, Mehta G. Intraoperative glove perforation - Single versus double gloving in protection against skin contamination. Postgrad Med J. 2001; 77(909):458–460. DOI: 10.1136/pmj.77.909.458.23. Yoo SJ, Lim YS, Kim MS. Incidence and risk factors for surgical glove perforation. J Korean Clin Nurs Res. 2010; 16(3):63–71.