J Korean Foot Ankle Soc.
2016 Sep;20(3):112-115. 10.14193/jkfas.2016.20.3.112.
Characteristics of Achilles Tendon Insertion on Posterior Aspect of the Calcaneus without Pathological Deformity in Adults: A Magnetic Resonance Imaging Study
- Affiliations
-
- 1Department of Orthopedic Surgery, Maryknoll Medical Center, Busan, Korea. daewon0809@naver.com
- 2Department of Orthopedic Surgery, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Orthopedic Surgery, Mega Hospital, Gimhae, Korea.
- KMID: 2351415
- DOI: http://doi.org/10.14193/jkfas.2016.20.3.112
Abstract
- PURPOSE
We aimed to investigate the safety zone for Achilles tendon insertion in the posterior aspect of the calcaneus via the use of magnetic resonance imaging (MRI) when planning for insertional Achilles tendinopathy.
MATERIALS AND METHODS
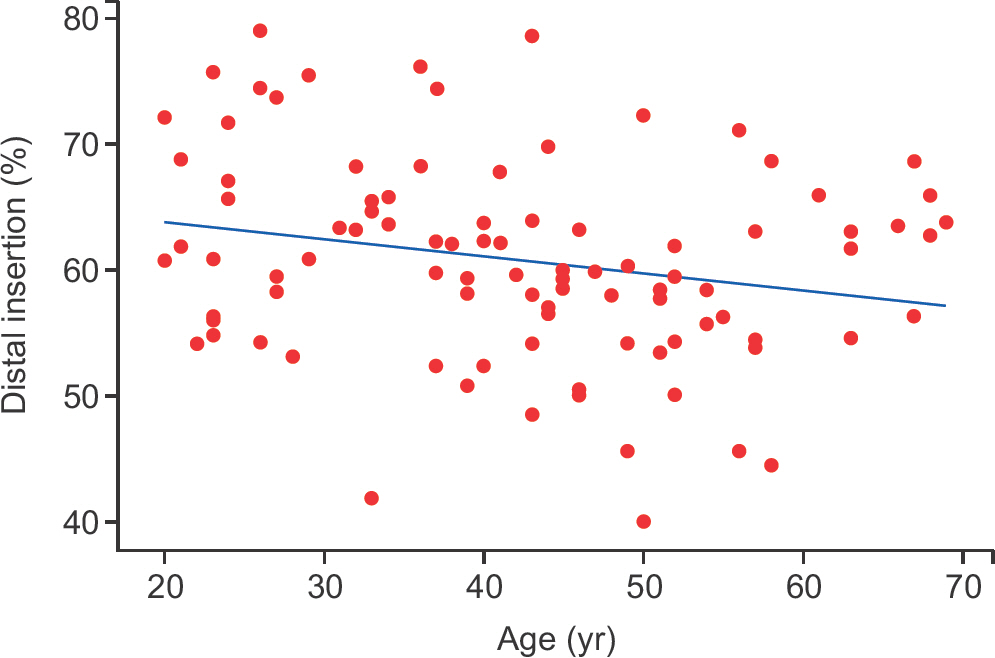
This study included 95 patients. The MRI of midsagittal plane of the ankle joint was used to measure the proximal and distal insertion point for the Achilles tendon in the posterior aspect of the calcaneus. Patients were divided into three groups according to the proportion of the distal insertion point out of the entire calcaneal length: the proximal, middle, and distal insertion groups.
RESULTS
The mean proximal and distal insertion points for the Achilles tendon were measured as 1.05 cm (0~2.11 cm) and 2.36 cm (1.60~2.93 cm), respectively. When the posterior aspect of the calcaneus was used as the reference plane, none of the patients was in the proximal insertion group, while 75 and 20 patients were in the middle and distal insertion groups, respectively. The insertion portion was longer in the distal insertion group (1.47±0.25 cm) than in the middle insertion group (1.27±0.35 cm). Statistically significant differences with respect to the length of the insertion portion were observed between the two groups (p=0.008).
CONCLUSION
Removal of more than 1 cm below the superior margin of the posterior calcaneus may be dangerous. An MRI study on the Achilles tendon of patients without hindfoot deformity or tendinopathy revealed various insertional characteristics. Preoperative MRI evaluation is safer than relying solely on the simple radiological assessment when planning for insertional Achilles tendinopathy.
MeSH Terms
Figure
Reference
-
1.Irwin TA. Current concepts review: insertional Achilles tendi-nopathy. Foot Ankle Int. 2010. 31:933–9.
Article2.Standring S. Gray’s anatomy: the anatomical basis of clinical practice. 39th ed.Edinburgh: Elsevier Churchill Livingstone;2005. p.1536.3.Marieb EN., Mallatt J. Human anatomy. Redwood City: Benjamin Cummings;1992. p. 285–7.4.Rohen JW., Yokochi C., Lütjen-Drecoll E., Romrell LJ. Color atlas of anatomy. 4th ed.Baltimore: Williams & Wilkins;1998. p. 462–3.5.Hamilton WG., Netter FH., Bean KJ. Clinical symposia: surgical anatomy of the foot and ankle. Summit: Ciba-Geigy;1985. p. 1–32.6.Chao W., Deland JT., Bates JE., Kenneally SM. Achilles tendon insertion: an in vitro anatomic study. Foot Ankle Int. 1997. 18:81–4.
Article7.Lohrer H., Arentz S., Nauck T., Dorn-Lange NV., Konerding MA. The achilles tendon insertion is crescent-shaped: an in vitro anatomic investigation. Clin Orthop Relat Res. 2008. 466:2230–7.8.Kim PJ., Martin E., Ballehr L., Richey JM., Steinberg JS. Variability of insertion of the achilles tendon on the calcaneus: an MRI study of younger subjects. J Foot Ankle Surg. 2011. 52:41–3.
Article9.Ahn SH., Cho HL., Hong SH., Wang TH. The results of the endoscopic decompression for the treatment of Haglund’s disease. J Korean Foot Ankle Soc. 2228. 12:197–202.10.van Dijk CN., van Dyk GE., Scholten PE., Kort NP. Endoscopic calcaneoplasty. Am J sports Med. 2001. 29:185–9.11.Jones DC., James SL. Partial calcaneal osteotomy for retrocalcaneal bursitis. Am J Sports Med. 1984. 12:72–3.12.Ortmann FW., McBryde AM. Endoscopic bony and soft-tissue decompression of the retrocalcaneal space for the treatment of Haglund deformity and retrocalcaneal bursitis. Foot Ankle Int. 2007. 28:149–53.
Article13.Frey C. Calcaneal prominence resection. Kitaoka HB, editor. editor.Master techniques in orthopaedic surgery: the foot and ankle. 2nd ed.Philadelphia: Lippincott Williams and Wilkins;2002. p. 357–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rupture of Achilles Tendon after Steroid Injection in Achilles Tendinitis (A Report of Five Cases)
- Reversed Tendon Sheath Wrapping on Indirect Rupture of Tendo Calcaneus
- Does Achilles Tendon Shortening Mean Pathologic Lesions?
- Heterotopic Ossification of a Partially Ruptured Achilles Tendon (A Case Report)
- Tendon Transfer on Deformity of the Foot