World J Mens Health.
2016 Aug;34(2):110-122. 10.5534/wjmh.2016.34.2.110.
A Systematic Review and Meta-Analysis of Functional Outcomes and Complications Following the Photoselective Vaporization of the Prostate and Monopolar Transurethral Resection of the Prostate
- Affiliations
-
- 1Department of Urology, Severance Hospital, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea. joouro@yuhs.ac
- 2Department of Urology, Gangnam Severance Hospital, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2349847
- DOI: http://doi.org/10.5534/wjmh.2016.34.2.110
Abstract
- PURPOSE
To perform a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing monopolar transurethral resection of the prostate (MTURP) and photoselective vaporization of the prostate (PVP) in order to provide the most up-to-date and reliable recommendations possible.
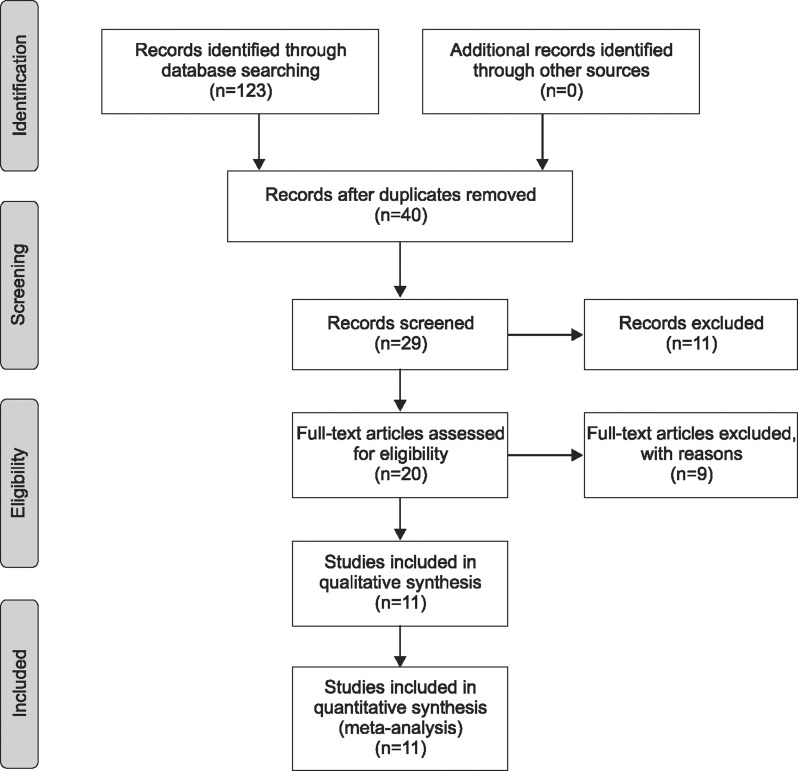
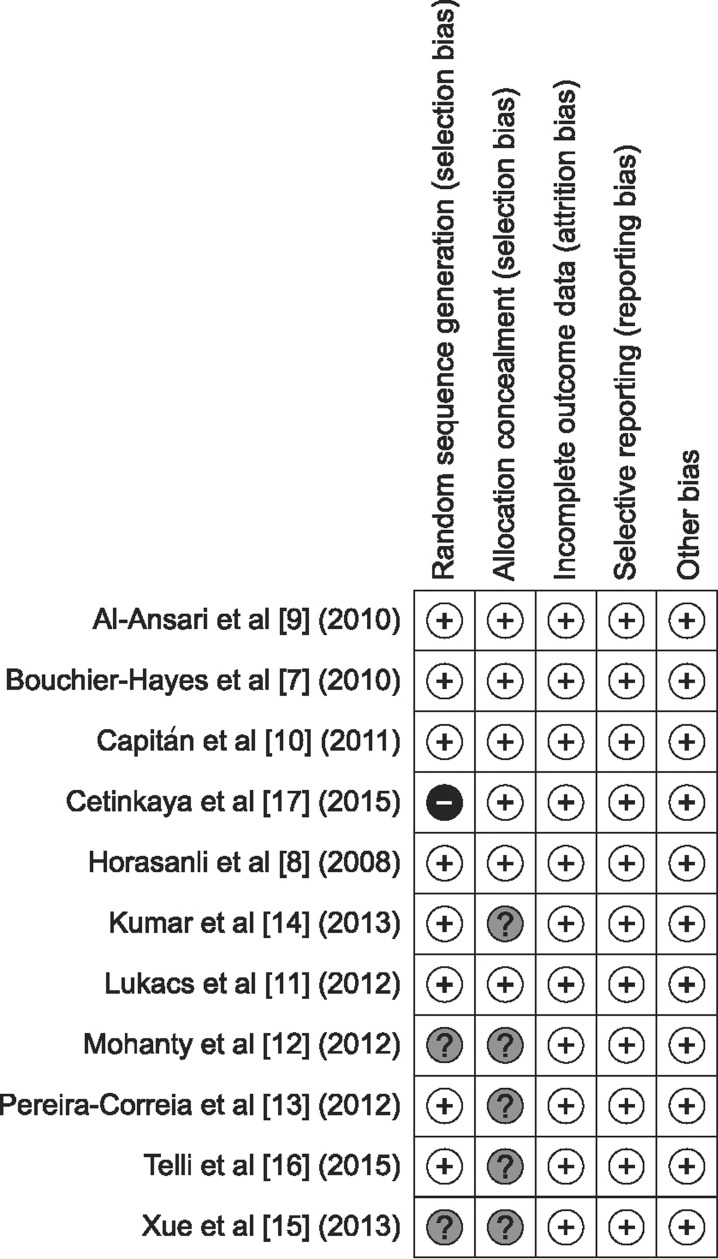
MATERIALS AND METHODS
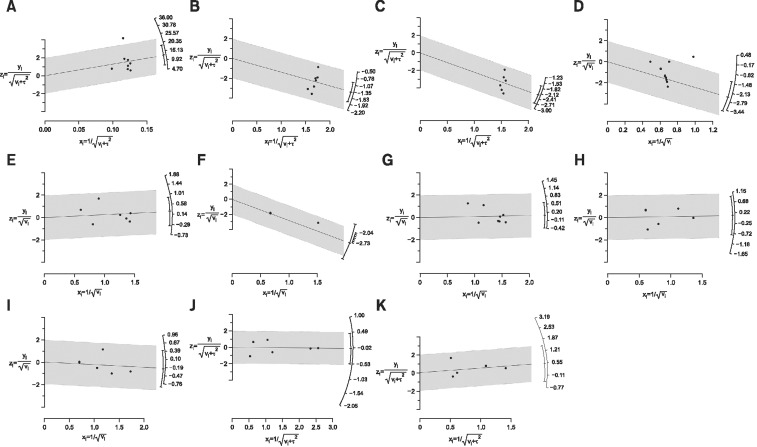
Relevant RCTs were identified from electronic databases for meta-analysis of the surgical outcomes and complications of MTURP and PVP. Meta-analytical comparisons were made using qualitative and quantitative syntheses. The outcome variables are presented as odds ratios with 95% confidence intervals (CIs).
RESULTS
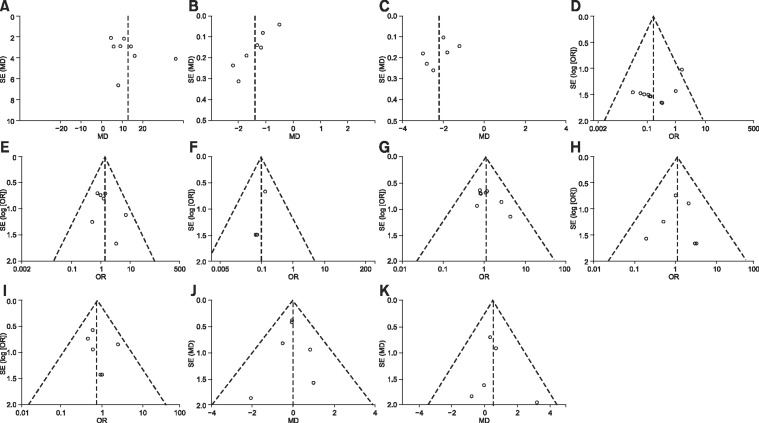
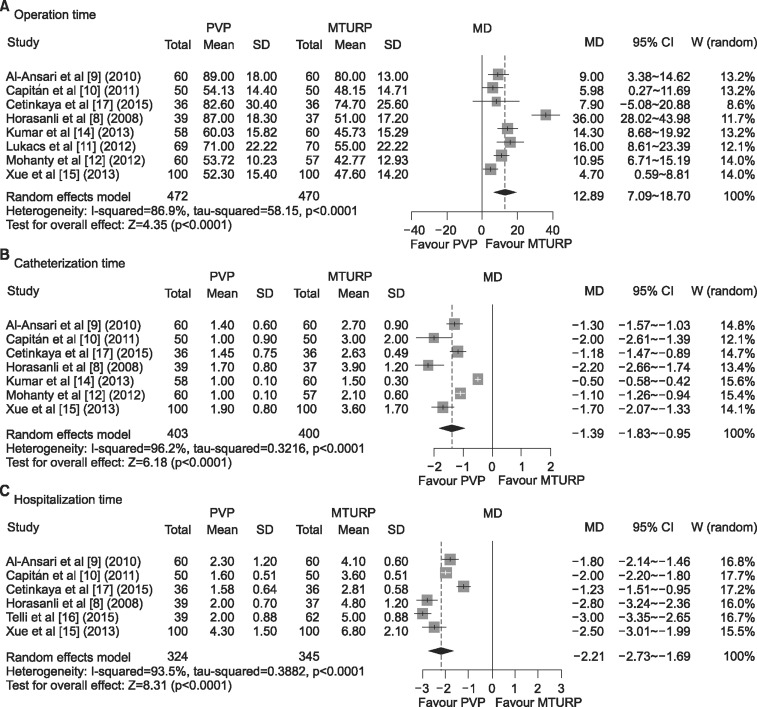
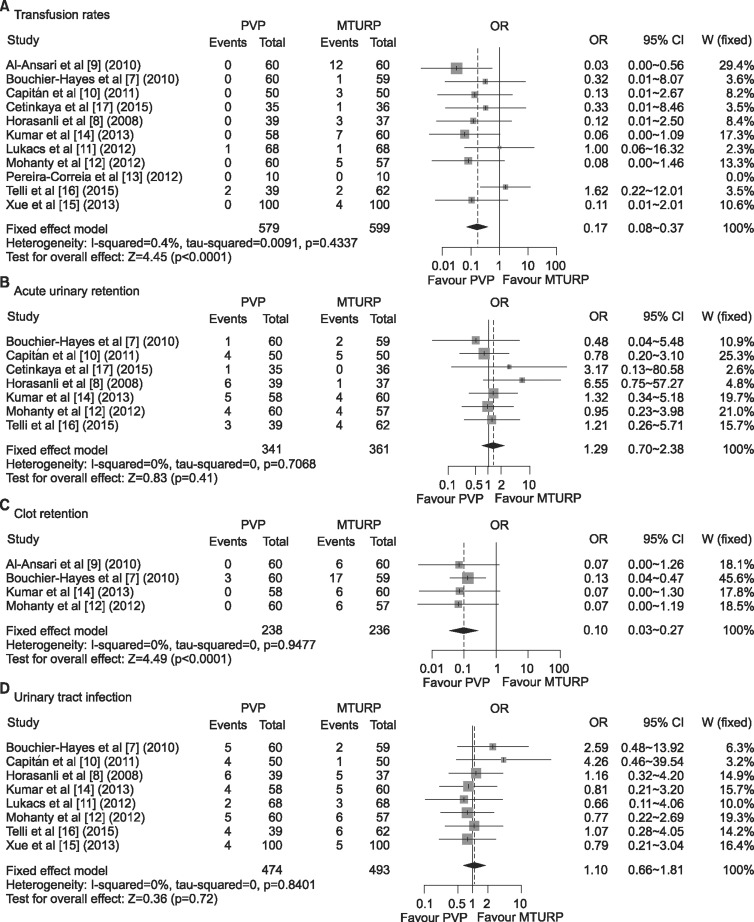
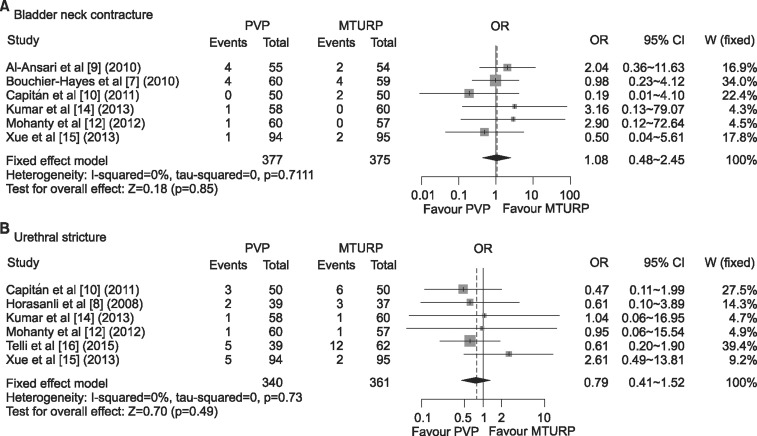
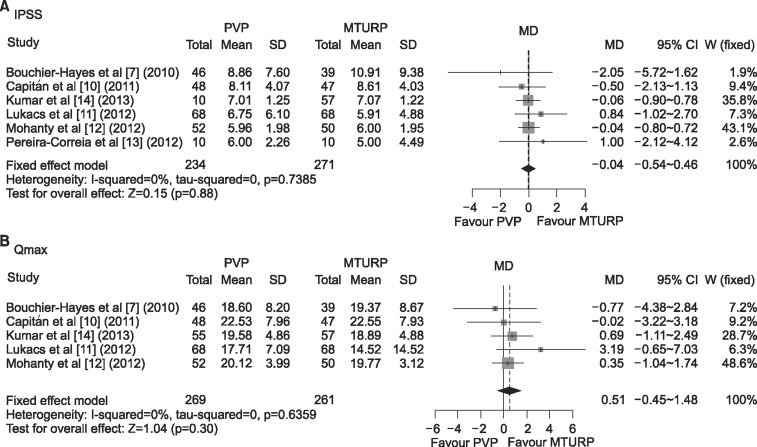
In total, 11 articles were included in this comparative analysis of PVP versus MTURP. Most of the recently published studies exhibited low risk in terms of quality assessment. MTURP was superior to PVP regarding operative time; however, with regard to catheterization and hospitalization time, the mean differences were -1.39 (95% CI=-1.83~-0.95, p<0.001) and -2.21 (95% CI=-2.73~-1.69, p<0.001), respectively, in favor of PVP. PVP was superior to MTURP with regard to transfusion rate and clot retention, but no statistically significant differences were found with regard to acute urinary retention and urinary tract infection. The long-term complications of bladder neck contracture and urethral stricture showed no statistically significant differences between PVP and MTURP. Long-term functional outcomes, including the International Prostate Symptom Score and maximum flow rate, likewise did not display statistically significant differences between PVP and MTURP.
CONCLUSIONS
Based on our findings, we believe that PVP should be considered as an alternative surgical procedure for treating male lower urinary tract symptoms secondary to benign prostatic hyperplasia.
MeSH Terms
Figure
Cited by 2 articles
-
Letter to the editor: Urethral strictures after bipolar transurethral resection of prostate may be linked to slow resection rate
Yu Seob Shin, Jong Kwan Park
Investig Clin Urol. 2018;59(1):66-67. doi: 10.4111/icu.2018.59.1.66.Changes in Erectile Function after Photoselective Vaporization of the Prostate with a 120-W GreenLight High-Performance System Laser: 2-Year Follow-Up
Juhyun Park, Sung Yong Cho, Min Chul Cho, Hyeon Jeong, Hwancheol Son
World J Mens Health. 2017;35(3):156-162. doi: 10.5534/wjmh.17027.
Reference
-
1. Martin SA, Haren MT, Marshall VR, Lange K, Wittert GA. Prevalence and factors associated with uncomplicated storage and voiding lower urinary tract symptoms in community-dwelling Australian men. World J Urol. 2011; 29:179–184. PMID: 20963421.
Article2. Chapple CR. Lower urinary tract symptoms suggestive of benign prostatic obstruction--triumph: design and implementation. Eur Urol. 2001; 39(Suppl 3):31–36. PMID: 11275740.3. Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravas S, Michel MC, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013; 64:118–140. PMID: 23541338.
Article4. Malek RS, Kuntzman RS, Barrett DM. Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes. J Urol. 2005; 174:1344–1348. PMID: 16145416.
Article5. Lee R, Gonzalez RR, Te AE. The evolution of photoselective vaporization prostatectomy (PVP): advancing the surgical treatment of benign prostatic hyperplasia. World J Urol. 2006; 24:405–409. PMID: 16699795.
Article6. Bachmann A, Ruszat R, Wyler S, Reich O, Seifert HH, Müller A, et al. Photoselective vaporization of the prostate: the basel experience after 108 procedures. Eur Urol. 2005; 47:798–804. PMID: 15925076.
Article7. Bouchier-Hayes DM, Van Appledorn S, Bugeja P, Crowe H, Challacombe B, Costello AJ. A randomized trial of photoselective vaporization of the prostate using the 80-W potassium-titanyl-phosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int. 2010; 105:964–969. PMID: 19912196.
Article8. Horasanli K, Silay MS, Altay B, Tanriverdi O, Sarica K, Miroglu C. Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology. 2008; 71:247–251. PMID: 18308094.
Article9. Al-Ansari A, Younes N, Sampige VP, Al-Rumaihi K, Ghafouri A, Gul T, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol. 2010; 58:349–355. PMID: 20605316.
Article10. Capitán C, Blázquez C, Martin MD, Hernández V, de la Peña E, Llorente C. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: a randomized clinical trial with 2-year follow-up. Eur Urol. 2011; 60:734–739. PMID: 21658839.
Article11. Lukacs B, Loeffler J, Bruyère F, Blanchet P, Gelet A, Coloby P, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: a multicenter randomized controlled trial. Eur Urol. 2012; 61:1165–1173. PMID: 22341632.
Article12. Mohanty NK, Vasudeva P, Kumar A, Prakash S, Jain M, Arora RP. Photoselective vaporization of prostate vs. transurethral resection of prostate: a prospective, randomized study with one year follow-up. Indian J Urol. 2012; 28:307–312. PMID: 23204660.
Article13. Pereira-Correia JA, de Moraes Sousa KD, Santos JB, de Morais Perpétuo D, Lopes-da-Silva LF, Krambeck RL, et al. GreenLight HPS™ 120-W laser vaporization vs transurethral resection of the prostate (<60 mL): a 2-year randomized double-blind prospective urodynamic investigation. BJU Int. 2012; 110:1184–1189. PMID: 22257240.14. Kumar A, Vasudeva P, Kumar N, Nanda B, Jha SK, Mohanty N. A prospective randomized comparative study of monopolar and bipolar transurethral resection of the prostate and photoselective vaporization of the prostate in patients who present with benign prostatic obstruction: a single center experience. J Endourol. 2013; 27:1245–1253. PMID: 23746047.
Article15. Xue B, Zang Y, Zhang Y, Yang D, Gao J, Sun C, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a prospective randomized trial. J Xray Sci Technol. 2013; 21:125–132. PMID: 23507858.
Article16. Telli O, Okutucu TM, Suer E, Burgu B, Gulpinar O, Yaman O, et al. A prospective, randomized comparative study of monopolar transurethral resection of the prostate versus photoselective vaporization of the prostate with GreenLight 120-W laser, in prostates less than 80 cc. Ther Adv Urol. 2015; 7:3–8. PMID: 25642290.17. Cetinkaya M, Onem K, Rifaioglu MM, Yalcin V. 980-Nm diode laser vaporization versus transurethral resection of the prostate for benign prostatic hyperplasia: randomized controlled study. Urol J. 2015; 12:2355–2361. PMID: 26571321.18. Chung JH, Lee SW. Assessing the quality of randomized controlled urological trials conducted by Korean medical institutions. Korean J Urol. 2013; 54:289–296. PMID: 23700493.
Article19. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994; 50:1088–1101. PMID: 7786990.
Article20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634. PMID: 9310563.
Article21. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID: 12958120.
Article22. Fleiss JL. Analysis of data from multiclinic trials. Control Clin Trials. 1986; 7:267–275. PMID: 3802849.
Article23. Galbraith RF. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med. 1988; 7:889–894. PMID: 3413368.
Article24. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007; 28:105–114. PMID: 16807131.
Article25. Teng J, Zhang D, Li Y, Yin L, Wang K, Cui X, et al. Photoselective vaporization with the green light laser vs transurethral resection of the prostate for treating benign prostate hyperplasia: a systematic review and meta-analysis. BJU Int. 2013; 111:312–323. PMID: 23145474.
Article26. Ding H, Du W, Lu ZP, Zhai ZX, Wang HZ, Wang ZP. Photoselective green-light laser vaporisation vs. TURP for BPH: meta-analysis. Asian J Androl. 2012; 14:720–725. PMID: 22902908.
Article27. Thangasamy IA, Chalasani V, Bachmann A, Woo HH. Photoselective vaporisation of the prostate using 80-W and 120-W laser versus transurethral resection of the prostate for benign prostatic hyperplasia: a systematic review with meta-analysis from 2002 to 2012. Eur Urol. 2012; 62:315–323. PMID: 22575913.
Article28. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479. PMID: 6206240.
Article29. McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011; 185:1793–1803. PMID: 21420124.
Article30. Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007; 94:1201–1208. PMID: 17729384.
Article31. Yin L, Teng J, Huang CJ, Zhang X, Xu D. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. J Endourol. 2013; 27:604–611. PMID: 23167266.
Article32. Li S, Zeng XT, Ruan XL, Weng H, Liu TZ, Wang X, et al. Holmium laser enucleation versus transurethral resection in patients with benign prostate hyperplasia: an updated systematic review with meta-analysis and trial sequential analysis. PLoS One. 2014; 9:e101615. PMID: 25003963.
Article33. Wendt-Nordahl G, Huckele S, Honeck P, Alken P, Knoll T, Michel MS, et al. 980-nm diode laser: a novel laser technology for vaporization of the prostate. Eur Urol. 2007; 52:1723–1728. PMID: 17611013.
Article34. Chen J, Wang M, Wang S, Sun P, Zhao Y, Zhang L, et al. 160-Watt lithium triboride laser vaporization versus transurethral resection of prostate: a prospective nonrandomized two-center trial. Urology. 2012; 79:650–654. PMID: 22386419.
Article35. Ouyang Y, Liu C, Guan W, Zhao Y, Xu Y, Wu Y. Impact of 160 W Greenlight laser vaporization of the prostate on erectile function: a prospective randomized controlled trial with 1-year follow-up. Photomed Laser Surg. 2014; 32:463–467. PMID: 25101536.
Article36. Castellan P, Castellucci R, Schips L, Cindolo L. Safety, efficacy and reliability of 180-W GreenLight laser technology for prostate vaporization: review of the literature. World J Urol. 2015; 33:599–607. PMID: 25647174.
Article37. Reich O, Bachmann A, Schneede P, Zaak D, Sulser T, Hofstetter A. Experimental comparison of high power (80 W) potassium titanyl phosphate laser vaporization and transurethral resection of the prostate. J Urol. 2004; 171:2502–2504. PMID: 15126885.
Article38. Choi YS, Bae WJ, Kim SJ, Kim KS, Cho HJ, Hong SH, et al. Efficacy and safety of 120-W GreenLight High-Performance System laser photo vaporization of the prostate: 3-year results with specific considerations. Prostate Int. 2013; 1:169–176. PMID: 24392442.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mini-Photoselective Vaporization of the Prostate for Difficult Intermittent Self-Catheterization
- Efficacy of Bipolar Transurethral Resection of the Prostate: Comparison with Standard Monopolar Transurethral Resection of the Prostate
- Comparison of Treatment Outcomes between Photoselective Vaporization and Transurethral Resection of the Prostate for Benign Prostatic Hyperplasia
- The Effect of 5-alpha Reductase Inhibitors on the Efficacy of Photoselective Vaporization of the Prostate with 120 W GreenLight HPS Laser
- Clinical Observation on Transurethral Resection of Prostate and Suprapubic Prostatectomy for Benign Prostatic Hypertrophy