J Korean Ophthalmol Soc.
2016 Aug;57(8):1241-1247. 10.3341/jkos.2016.57.8.1241.
Scleral Lens Application for Preventing Corneal Edema During Vitrectomy
- Affiliations
-
- 1Department of Ophthalmology, Dong-A University College of Medicine, Busan, Korea. wjeye@dau.ac.kr
- KMID: 2349070
- DOI: http://doi.org/10.3341/jkos.2016.57.8.1241
Abstract
- PURPOSE
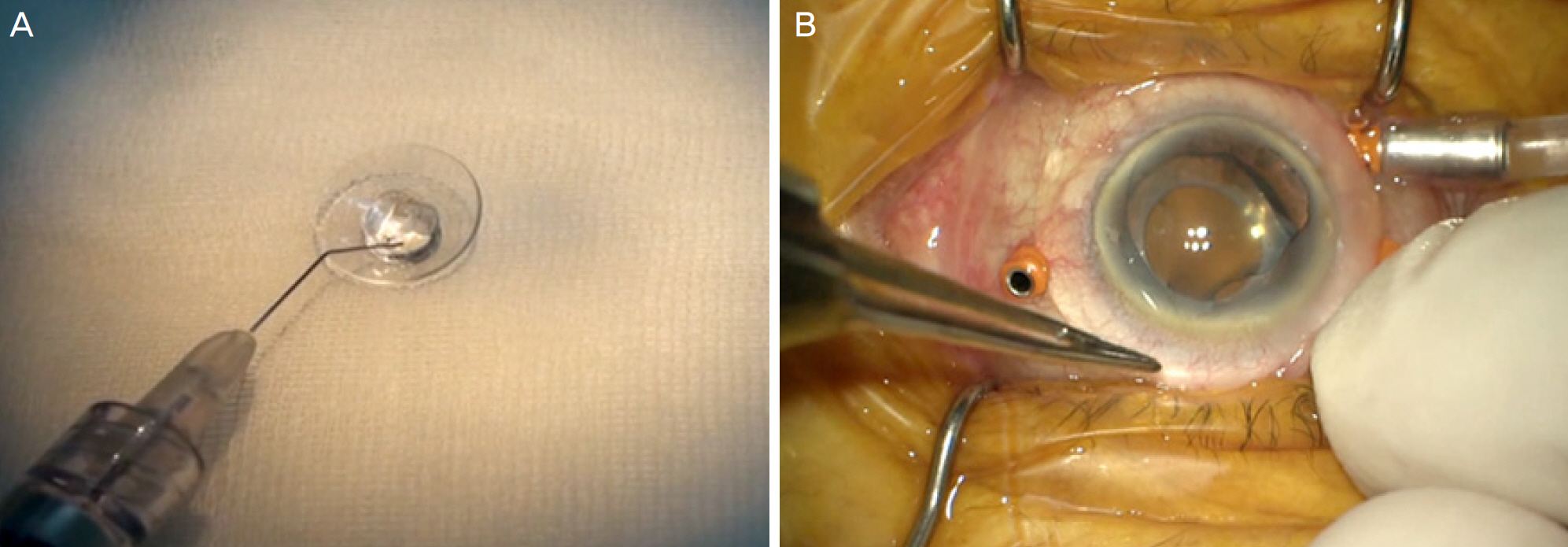
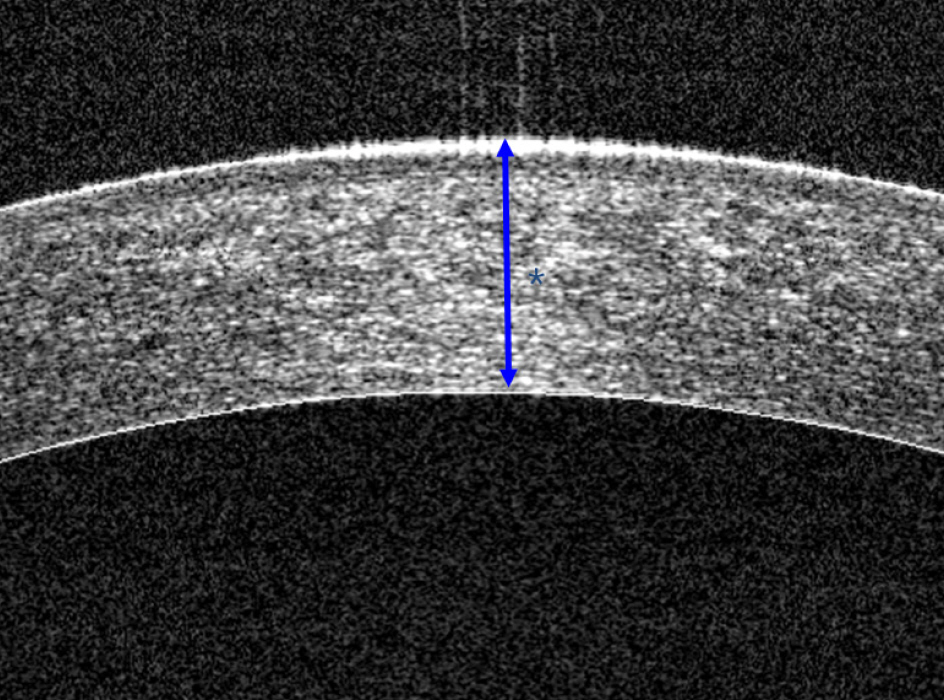
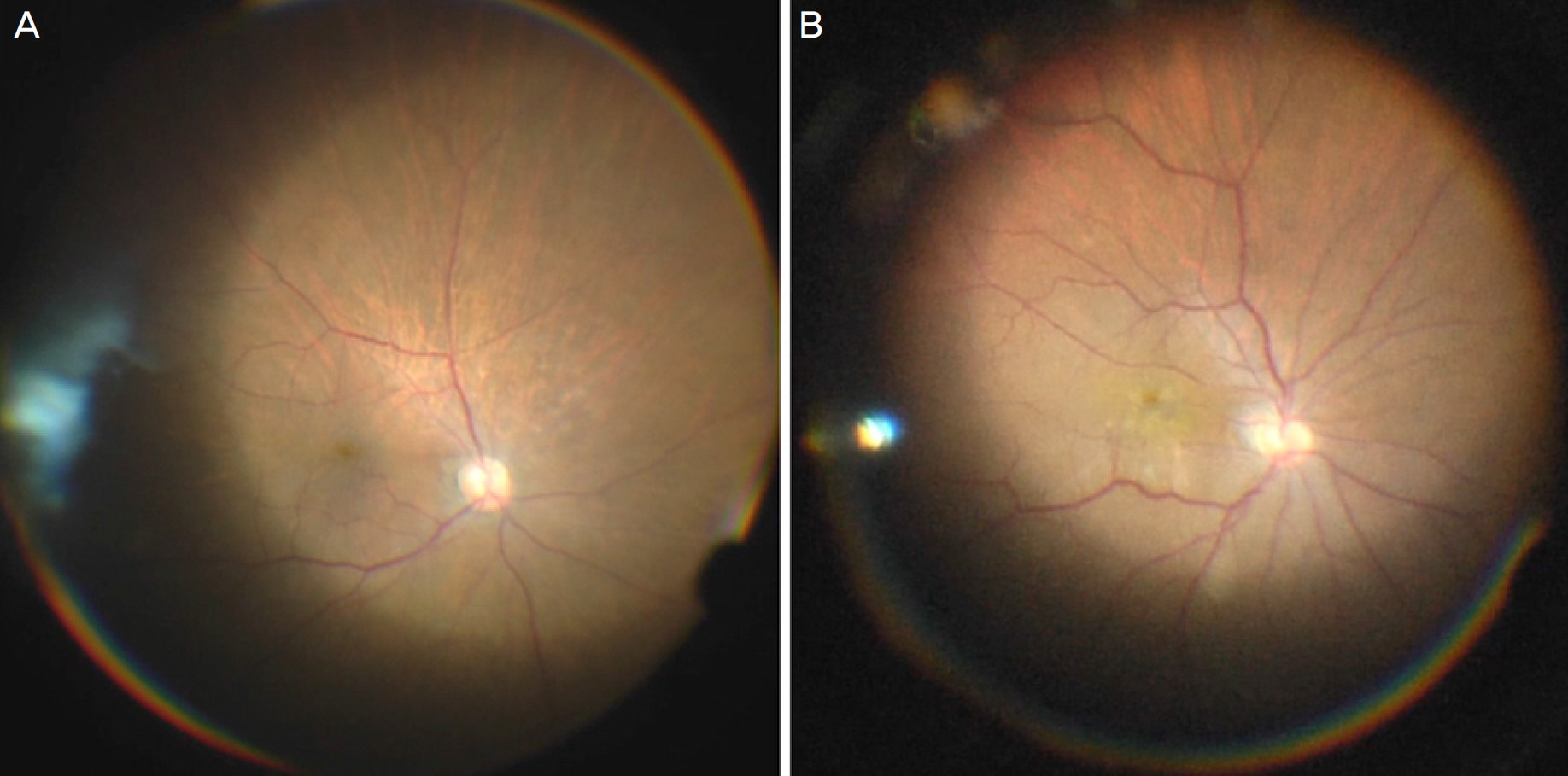
To analyze the effect of scleral lens application for preventing corneal edema during vitrectomy on postoperative corneal status using anterior segment OCT (RTVue 100, Optovue, Fremont, CA, USA).
METHODS
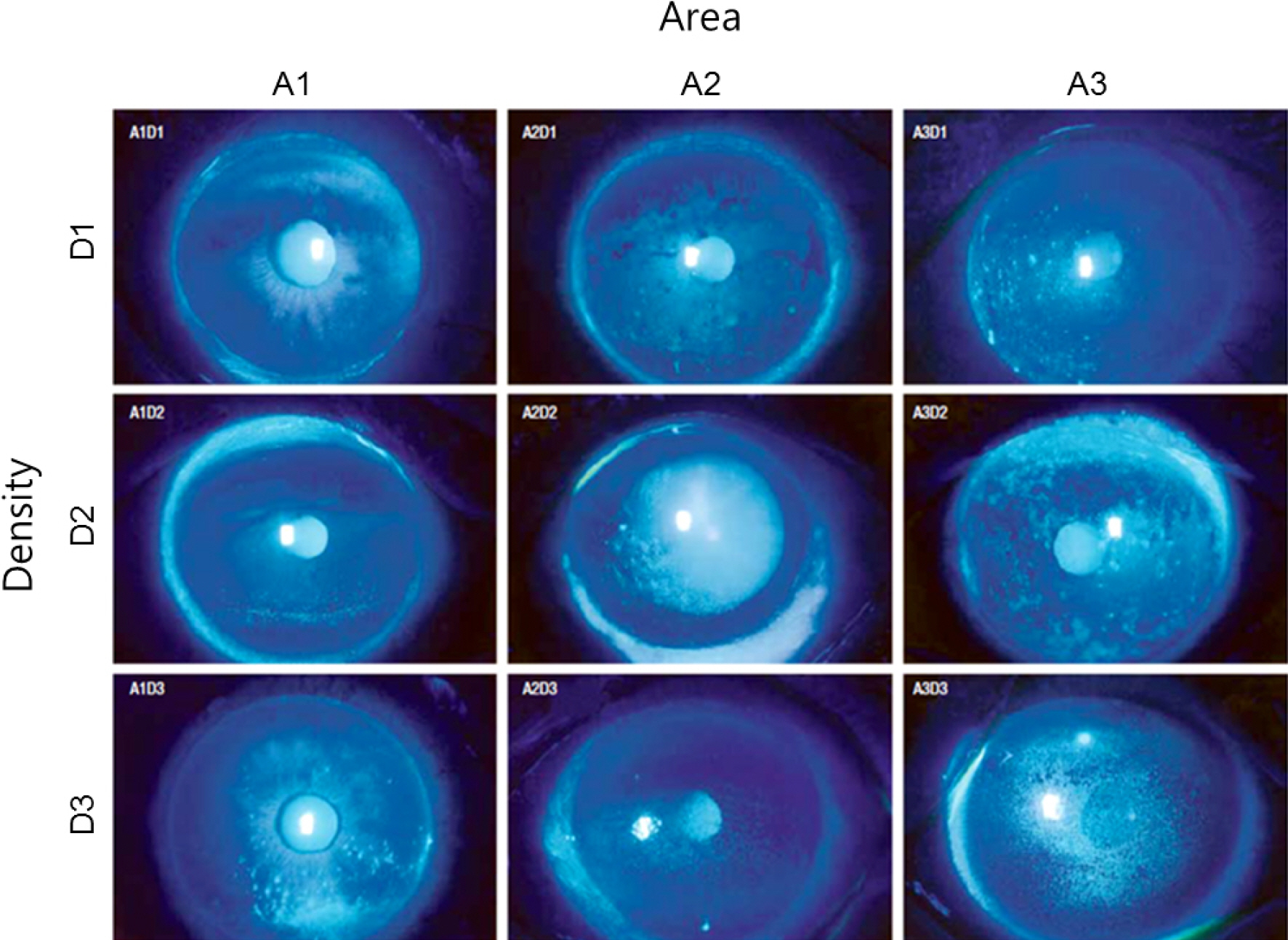
The medical records of 42 eyes (42 patients) who underwent total vitrectomy with no appreciable corneal disease between November 2014 and June 2015 were retrospectively reviewed. Evaluations were performed at 1 day, 1 week, and 1 month after total vitrectomy. Corneal status was noted at every follow-up visit using anterior segment OCT. An analysis was performed to define the changes in corneal status in association with scleral lens application during the surgery.
RESULTS
18 of 42 eyes were treated with a scleral lens during total vitrectomy. The corneal thickness increased after vitrectomy in all cases. The mean corneal thickness increment was 23.9 ± 9.7 µm in the scleral lens group and 43.0 ± 19.5 µm in the non-scleral lens group at 1 day after vitrectomy (p < 0.001). At 1 week after vitrectomy, the mean corneal thickness increment was 8.1 ± 7.2 µm in the scleral lens group and 32.3 ± 19.2 µm in the non-scleral lens group (p < 0.001). The difference in superficial punctate keratitis grade between the two groups was not statistically significant.
CONCLUSION
Scleral lens application during vitrectomy seems to prevent postoperative corneal edema. More cases and a longer period of study is needed to draw definitive conclusions.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Perry HD, Foulks GN, Thoft RA, Tolentino FI. Corneal complications after closed vitrectomy through the pars plana. Arch Ophthalmol. 1978; 96:1401–3.
Article2. Chiambo S, Baílez Fidalgo C, Pastor Jimeno JC, et al. Corneal abdominal complications after vitrectomy: a retrospective study. Arch Soc Esp Oftalmol. 2004; 79:155–61.3. Kamei M, Matsumura N, Sakaguchi H, et al. Commercially abdominal rigid gas-permeable contact lens for protecting the cornea from drying during vitrectomy with a wide viewing system. Clin Ophthalmol. 2012; 6:1321–4.4. Spencer R, Newsome DA, Schepens CL. Limited superficial abdominal to improve corneal clarity during closed vitrectomy. Am J Ophthalmol. 1980; 89:137–8.5. Tosi GM, Marigliani D, Bacci T, et al. Impact of intraoperative abdominal hydroxypropyl methylcellulose 2% versus sodium hyaluronate 1.2% on corneal reepithelialization after intentional epithelial abdominal during vitrectomy. Cornea. 2014; 33:942–5.6. Schornack MM, Pyle J, Patel SV. Scleral lenses in the management of ocular surface disease. Ophthalmology. 2014; 121:1398–405.
Article7. Miyata K, Amano S, Sawa M, Nishida T. A novel grading method for superficial punctate keratopathy magnitude and its correlation with corneal epithelial permeability. Arch Ophthalmol. 2003; 121:1537–9.
Article8. Romero-Rangel T, Stavrou P, Cotter J, et al. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol. 2000; 130:25–32.
Article9. Rosenthal P, Cotter J. The Boston Scleral Lens in the management of severe ocular surface disease. Ophthalmol Clin North Am. 2003; 16:89–93.
Article10. Rosenthal P, Croteau A. Fluidventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular abdominal disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens. 2005; 31:130–4.11. Rosenthal P, Cotter JM, Baum J. Treatment of persistent corneal epithelial defect with extended wear of a fluidventilated gas-per-meable scleral contact lens. Am J Ophthalmol. 2000; 130:33–41.
Article12. Jacobs DS, Rosenthal P. Boston scleral lens prosthetic device for treatment of severe dry eye in chronic graft-versus-host disease. Cornea. 2007; 26:1195–9.
Article13. Schornack MM, Baratz KH, Patel SV, Maguire LJ. Jupiter scleral lenses in the management of chronic graft versus host disease. Eye Contact Lens. 2008; 34:302–5.
Article14. Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: the expanding role. Cornea. 2005; 24:269–77.15. van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral contact lenses: a review. Cont Lens Anterior Eye. 2014; 37:240–50.
Article16. Dalton K, Sorbara L. Fitting an MSD (mini scleral design) rigid contact lens in advanced keratoconus with INTACS. Cont Lens Anterior Eye. 2011; 34:274–81.
Article17. Alipour F, Behrouz MJ, Samet B, et al. Mini-scleral lenses in the visual rehabilitation of patients after penetrating keratoplasty and deep lamellar anterior keratoplasty. Cont Lens Anterior Eye. 2015; 38:54–8.
Article18. Segal O, Barkana Y, Hourovitz D, et al. Scleral contact lenses may help where other modalities fail. Cornea. 2003; 22:308–10.
Article19. Chung H, Tolentino FI, Cajita VN, et al. Reevaluation of corneal complications after closed vitrectomy. Arch Ophthalmol. 1988; 106:916–9.
Article20. Friberg TR, Doran DL, Lazenby FL. The effect of vitreous and abdominall surgery on corneal endothelial cell density. Ophthalmology. 1984; 91:1166–9.21. Goezinne F, Nuijts RM, Liem AT, et al. Corneal endothelial cell density after vitrectomy with silicone oil for complex retinal detachments. Retina. 2014; 34:228–36.
Article22. Farrahi F, Feghhi M, Ostadian F, Alivand A. Pars plana vitrectomy and silicone oil injection in phakic and pseudophakic eyes; corneal endothelial changes. J Ophthalmic Vis Res. 2014; 9:310–3.23. Matsuda M, Tano Y, Inaba M, Manabe R. Corneal endothelial cell damage associated with intraocular gas tamponade during pars abdominal vitrectomy. Jpn J Ophthalmol. 1986; 30:324–9.24. Watanabe A, Shibata T, Takashina H, et al. Changes in corneal thickness following vitreous surgery. Clin Ophthalmol. 2012; 6:1293–6.
Article25. Chen HF, Yeung L, Yang KJ, Sun CC. Persistent corneal epithelial defect after pars plana vitrectomy. Retina. 2016; 36:148–55.
Article26. Hiraoka M, Amano S, Oshika T, et al. Factors contributing to abdominal complications after vitrectomy in diabetic patients. Jpn J Ophthalmol. 2001; 45:492–5.27. Foulks GN, Thoft RA, Perry HD, Tolentino FI. Factors related to corneal epithelial complications after closed vitrectomy in diabetics. Arch Ophthalmol. 1979; 97:1076–8.
Article28. Matsumura T, Takamura Y, Tomomatsu T, et al. Changes in matrix metalloproteinases in diabetes patients' tears after vitrectomy and the relationship with corneal epithelial disorder. Invest Ophthalmol Vis Sci. 2015; 56:3559–64.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guide for Successful Scleral Lens Fitting
- Perfluoro-N-octane as Postoperative Vitreous Substitutes in Retinal Detachment: A Case Report
- Clinical Use of Mini-Scleral Contact Lens in Ocular Surface Diseases
- Transscleral Fixation of Intraocular Lens Using the Triple Cow-Hitch Method
- The Changes of Corneal Curvature after Scleral Resection