Korean J Ophthalmol.
2014 Dec;28(6):451-459. 10.3341/kjo.2014.28.6.451.
Changing Trends in Surgery for Retinal Detachment in Korea
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. swkang@skku.edu
- 2Doctor Lee's Clinic, Suwon, Korea.
- KMID: 2345821
- DOI: http://doi.org/10.3341/kjo.2014.28.6.451
Abstract
- PURPOSE
To analyze trends in rhegmatogenous retinal detachment (RRD) surgery among the members of the Korean Retina Society from 2001 to 2013.
METHODS
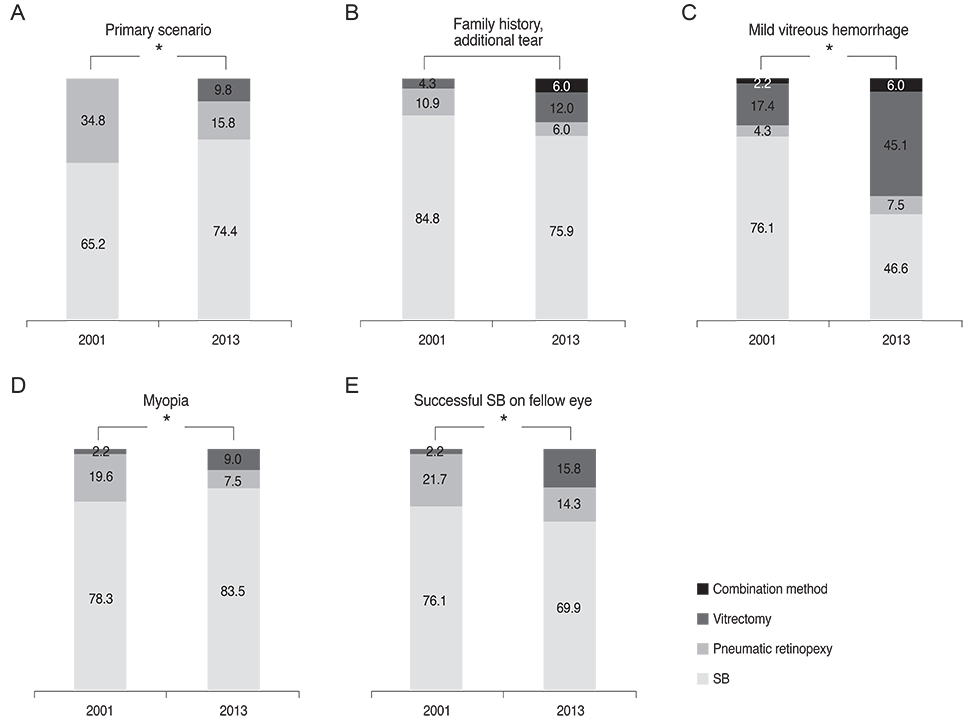
In 2013, surveys were conducted by email and post to investigate the current practice patterns regarding RRD treatment. Questions included how surgeons would manage six cases of hypothetical RRD. Results were compared to those reported in 2001.
RESULTS
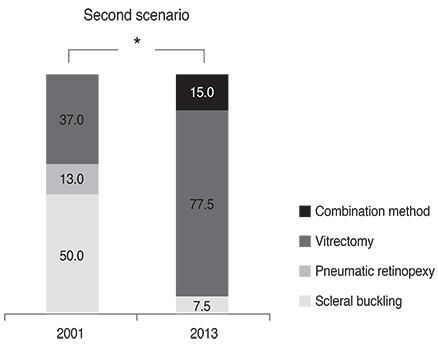
A total of 133 members (60.7%) in 2013 and 46 members(79.3%) in 2001 responded to the survey. Preference for pneumatic retinopexy has decreased in uncomplicated primary RRD (p = 0.004). More respondents in 2013 selected vitrectomy as the primary procedure when mild vitreous hemorrhage (p = 0.001), myopia (p = 0.044) and history of successful scleral buckling on the fellow eye (p = 0.044) were added to the primary scenario. Vitrectomy was over twice as popular in cases of pseudophakic, macula-off RRD with posterior capsular opacity (p = 0.001).
CONCLUSIONS
For RRD with myopia, pseudophakia and media opacity, surgical interventions over the last decade have drastically shifted from scleral buckling and pneumatic retinopexy to vitrectomy.
Keyword
MeSH Terms
-
Endotamponade/trends
Female
Health Care Surveys
Humans
Male
Middle Aged
Ophthalmologic Surgical Procedures/*trends
Ophthalmology/organization & administration
Practice Patterns, Physicians'/*trends
Republic of Korea
Retinal Detachment/*surgery
Scleral Buckling/trends
Societies, Medical
Surveys and Questionnaires
Vitrectomy/trends
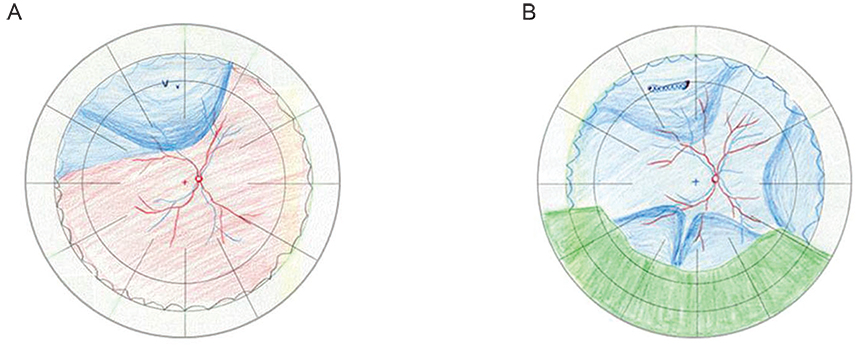
Figure
Reference
-
1. Schwartz SG, Flynn HW. Primary retinal detachment: scleral buckle or pars plana vitrectomy? Curr Opin Ophthalmol. 2006; 17:245–250.2. Escoffery RF, Olk RJ, Grand MG, Boniuk I. Vitrectomy without scleral buckling for primary rhegmatogenous retinal detachment. Am J Ophthalmol. 1985; 99:275–281.3. Campo RV, Sipperley JO, Sneed SR, et al. Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology. 1999; 106:1811–1815.4. Gartry DS, Chignell AH, Franks WA, Wong D. Pars plana vitrectomy for the treatment of rhegmatogenous retinal detachment uncomplicated by advanced proliferative vitreoretinopathy. Br J Ophthalmol. 1993; 77:199–203.5. Azad RV, Chanana B, Sharma YR, Vohra R. Primary vitrectomy versus conventional retinal detachment surgery in phakic rhegmatogenous retinal detachment. Acta Ophthalmol Scand. 2007; 85:540–545.6. Heimann H, Bartz-Schmidt KU, Bornfeld N, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007; 114:2142–2154.7. Ahmadieh H, Moradian S, Faghihi H, et al. Anatomic and visual outcomes of scleral buckling versus primary vitrectomy in pseudophakic and aphakic retinal detachment: six-month follow-up results of a single operation: report no. 1. Ophthalmology. 2005; 112:1421–1429.8. Brazitikos PD, Androudi S, Christen WG, Stangos NT. Primary pars plana vitrectomy versus scleral buckle surgery for the treatment of pseudophakic retinal detachment: a randomized clinical trial. Retina. 2005; 25:957–964.9. Snyder WB, Bloome MA, Birch DG. Pneumatic retinopexy versus scleral buckle: preferences of Vitreous Society members, 1990. Retina. 1992; 12:43–45.10. Benson WE, Chan P, Sharma S, et al. Current popularity of pneumatic retinopexy. Retina. 1999; 19:238–241.11. Kang SW, Kim SW. The Korean Retina Society. Preferences for treatment modalities of simple rhegmatogenous tetinal detachment in Korea. J Korean Ophthalmol Soc. 2002; 43:1179–1185.12. Minihan M, Tanner V, Williamson TH. Primary rhegmatogenous retinal detachment: 20 years of change. Br J Ophthalmol. 2001; 85:546–548.13. Falkner-Radler CI, Myung JS, Moussa S, et al. Trends in primary retinal detachment surgery: results of a Bicenter study. Retina. 2011; 31:928–936.14. Tornambe PE. Pneumatic retinopexy: the evolution of case selection and surgical technique: a twelve-year study of 302 eyes. Trans Am Ophthalmol Soc. 1997; 95:551–578.15. Hilton GF, Tornambe PE, Grizzard WS. Results of a temporary balloon buckle in the treatment of 500 retinal detachments and a comparison with pneumatic retinopexy. Am J Ophthalmol. 1989; 108:612–614.16. Zaidi AA, Alvarado R, Irvine A. Pneumatic retinopexy: success rate and complications. Br J Ophthalmol. 2006; 90:427–428.17. Chan CK, Lin SG, Nuthi AS, Salib DM. Pneumatic retinopexy for the repair of retinal detachments: a comprehensive review (1986-2007). Surv Ophthalmol. 2008; 53:443–478.18. Day S, Grossman DS, Mruthyunjaya P, et al. One-year outcomes after retinal detachment surgery among medicare beneficiaries. Am J Ophthalmol. 2010; 150:338–345.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Retinal Detachment with Equatorial Scleral Staphyloma
- A Case of Retinal Detachment with Equatorial Scleral Staphyloma
- Comparision of Clinical Findings between Phakic Retinal and Pseudophakic Retinal Detachment
- Three Cases of Pneumoretinopexy for Rhegmatogenous Retinal Detachment by Multiple Retinal Tears over 1 Hour in Distance
- Pathology of Rhegmatogenous Retinal Detachment