J Korean Soc Radiol.
2011 Nov;65(5):495-503.
Comparative Study between Digital Tomosynthesis and Endoscopic Retrograde Cholangiopancreatography for the Evaluation of Common Bile Duct Stones: Focus on Detection and Stone Conspicuity
- Affiliations
-
- 1Department of Radiology and Medical Research Institute, School of Medicine, Ewha Womans University, Seoul, Korea. bbaek@ewha.ac.kr
- 2Department of Internal Medicine and Medical Research Institute, School of Medicine, Ewha Womans University, Seoul, Korea.
Abstract
- PURPOSE
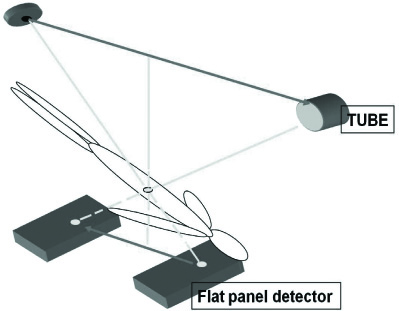
To compare digital tomosynthesis with endoscopic retrograde cholangiopancreatography (ERCP) for the evaluation of common bile duct (CBD) stones as a complementary diagnostic tool.
MATERIALS AND METHODS
Ninety six consecutive patients clinically suspected of having CBD stones underwent ERCP and digital tomosynthesis over 22 months, from December, 2008 to May, 2010. Fourteen patients were excluded. Therefore 82 patients were included in this study. The images were retrospectively reviewed to compare the results with the final analysis based on the consensus of two abdominal radiologists. An evaluation of the presence of CBD stones was followed by a determination of the margins for the stones, scored with a five-point conspicuity scale.
RESULTS
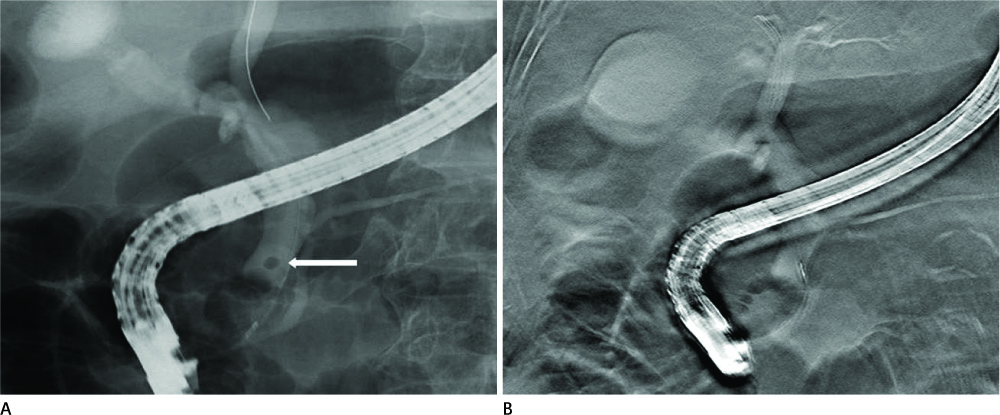
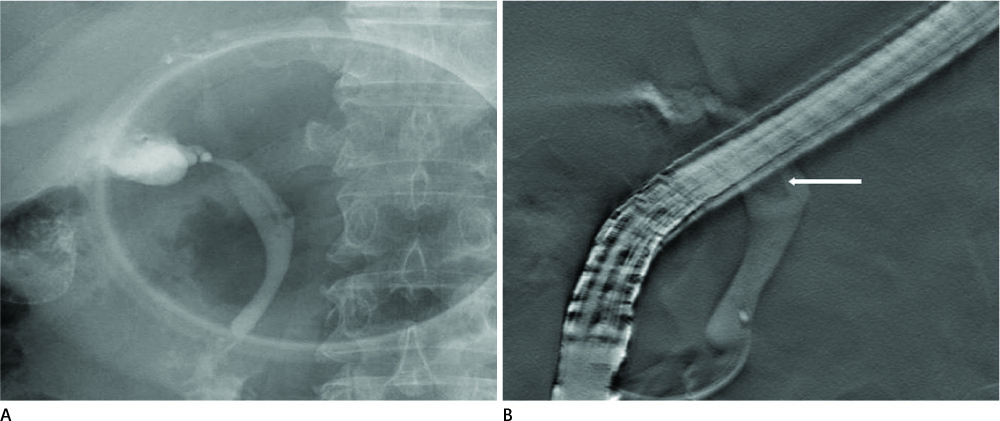
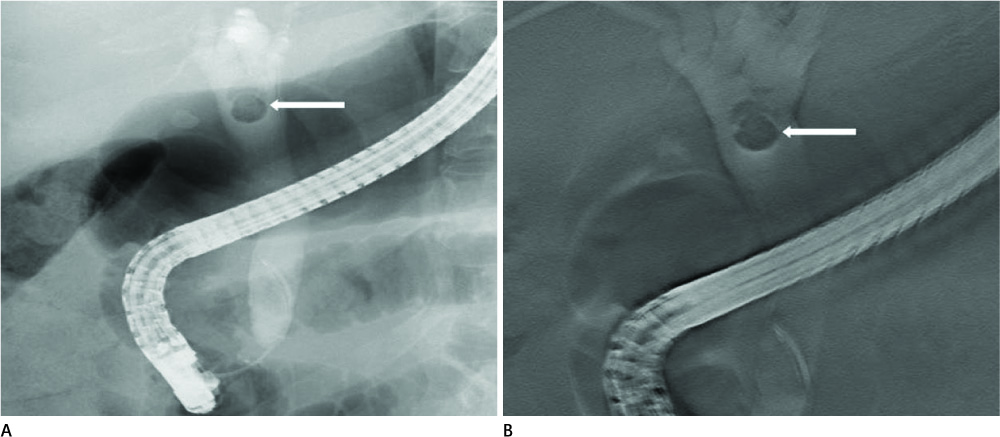
Among the 82 patients, 54 collectively had 89 CBD stones and 28 had no stones. The sensitivity and specificity for the detection of CBD stones were 91.0% and 80.6% for ERCP, 92.1% and 93.5% for digital tomosynthesis, respectively. The average score was 3.29 for ERCP and 3.89 for digital tomosynthesis in 77 similar detected stones. Digital tomosynthesis demonstrated significantly better conspicuity than ERCP (p = 0.001).
CONCLUSION
Digital tomosynthesis is an effective and complementary diagnostic method for the evaluation of CBD stones.
MeSH Terms
Figure
Reference
-
1. Dobbins JT 3rd, Godfrey DJ. Digital x-ray tomosynthesis: current state of the art and clinical potential. Phys Med Biol. 2003; 48:R65–R106.2. Vikgren J, Zachrisson S, Svalkvist A, Johnsson AA, Boijsen M, Flinck A, et al. Comparison of chest tomosynthesis and chest radiography for detection of pulmonary nodules: human observer study of clinical cases. Radiology. 2008; 249:1034–1041.3. Tingberg A. X-ray tomosynthesis: a review of its use for breast and chest imaging. Radiat Prot Dosimetry. 2010; 139:100–107.4. Dobbins JT 3rd, McAdams HP. Chest tomosynthesis: technical principles and clinical update. Eur J Radiol. 2009; 72:244–251.5. Dobbins JT 3rd, McAdams HP, Godfrey DJ, Li CM. Digital tomosynthesis of the chest. J Thorac Imaging. 2008; 23:86–92.6. Pasanen P, Partanen K, Pikkarainen P, Alhava E, Pirinen A, Janatuinen E. Ultrasonography, CT, and ERCP in the diagnosis of choledochal stones. Acta Radiol. 1992; 33:53–56.7. Pickuth D, Spielmann RP. Detection of choledocholithiasis: comparison of unenhanced spiral CT, US, and ERCP. Hepatogastroenterology. 2000; 47:1514–1517.8. Rickes S, Treiber G, Mönkemüller K, Peitz U, Csepregi A, Kahl S, et al. Impact of the operator's experience on value of high-resolution transabdominal ultrasound in the diagnosis of choledocholithiasis: a prospective comparison using endoscopic retrograde cholangiography as the gold standard. Scand J Gastroenterol. 2006; 41:838–843.9. Stott MA, Farrands PA, Guyer PB, Dewbury KC, Browning JJ, Sutton R. Ultrasound of the common bile duct in patients undergoing cholecystectomy. J Clin Ultrasound. 1991; 19:73–76.10. Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005; 54:271–275.11. Breen DJ, Nicholson AA. The clinical utility of spiral CT cholangiography. Clin Radiol. 2000; 55:733–739.12. Persson A, Dahlström N, Smedby O, Brismar TB. Three-dimensional drip infusion CT cholangiography in patients with suspected obstructive biliary disease: a retrospective analysis of feasibility and adverse reaction to contrast material. BMC Med Imaging. 2006; 6:1.13. Nilsson U. Adverse reactions to iotroxate at intravenous cholangiography. A prospective clinical investigation and review of the literature. Acta Radiol. 1987; 28:571–557.14. Griffin N, Wastle ML, Dunn WK, Ryder SD, Beckingham IJ. Magnetic resonance cholangiopancreatography versus endoscopic retrograde cholangiopancreatography in the diagnosis of choledocholithiasis. Eur J Gastroenterol Hepatol. 2003; 15:809–813.15. Kim TK, Kim BS, Kim JH, Ha HK, Kim PN, Kim AY, et al. Diagnosis of intrahepatic stones: superiority of MR cholangiopancreatography over endoscopic retrograde cholangiopancreatography. AJR Am J Roentgenol. 2002; 179:429–434.16. Stiris MG, Tennøe B, Aadland E, Lunde OC. MR cholangiopancreaticography and endoscopic retrograde cholangiopancreaticography in patients with suspected common bile duct stones. Acta Radiol. 2000; 41:269–272.17. Kats J, Kraai M, Dijkstra AJ, Koster K, Ter Borg F, Hazenberg HJ, et al. Magnetic resonance cholangiopancreaticography as a diagnostic tool for common bile duct stones: a comparison with ERCP and clinical follow-up. Dig Surg. 2003; 20:32–37.18. Kessler RE, Falkenstein DB, Clemett AR, Zimmon DS. Indications, clinical value and complications of endoscopic retrograde cholangiopancreatography. Surg Gynecol Obstet. 1976; 142:865–870.19. Silviera ML, Seamon MJ, Porshinsky B, Prosciak MP, Doraiswamy VA, Wang CF, et al. Complications related to endoscopic retrograde cholangiopancreatography: a comprehensive clinical review. J Gastrointestin Liver Dis. 2009; 18:73–82.20. Rieger R, Wayand W. Yield of prospective, noninvasive evaluation of the common bile duct combined with selective ERCP/sphincterotomy in 1390 consecutive laparoscopic cholecystectomy patients. Gastrointest Endosc. 1995; 42:6–12.21. Vitale GC, Larson GM, Wieman TJ, Cheadle WG, Miller FB. The use of ERCP in the management of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 1993; 7:9–11.22. Cotton PB. Endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. Am J Surg. 1993; 165:474–478.23. Shiozawa S, Kim DH, Usui T, Tsuchiya A, Masuda T, Inose S, et al. Indication of endoscopic retrograde cholangiography by noninvasive predictive factors of common bile duct stones before laparoscopic cholecystectomy: a prospective clinical study. Surg Laparosc Endosc Percutan Tech. 2011; 21:28–32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Yellow-to-white and Black Extrahepatic Bile Duct Stones
- The Endoscopic Management of Common Bile Duct Stones
- Cholelithiasis Fortunately Removed by Endoscopic Retrograde Cholangiopancreatography
- Ultrasonographic findings of intrahepatic bile duct stone
- A Common Bile Duct Web in Association with Bile Duct Stone Treated with Balloon Dilatation