Korean Circ J.
2016 Jul;46(4):574-579. 10.4070/kcj.2016.46.4.574.
Spontaneous Transition of Double Tachycardias with Atrial Fusion in a Patient with Wolff-Parkinson-White Syndrome
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, School of Medicine, Dankook University, Cheonan, Korea. mel_lee@dankook.ac.kr
- KMID: 2344435
- DOI: http://doi.org/10.4070/kcj.2016.46.4.574
Abstract
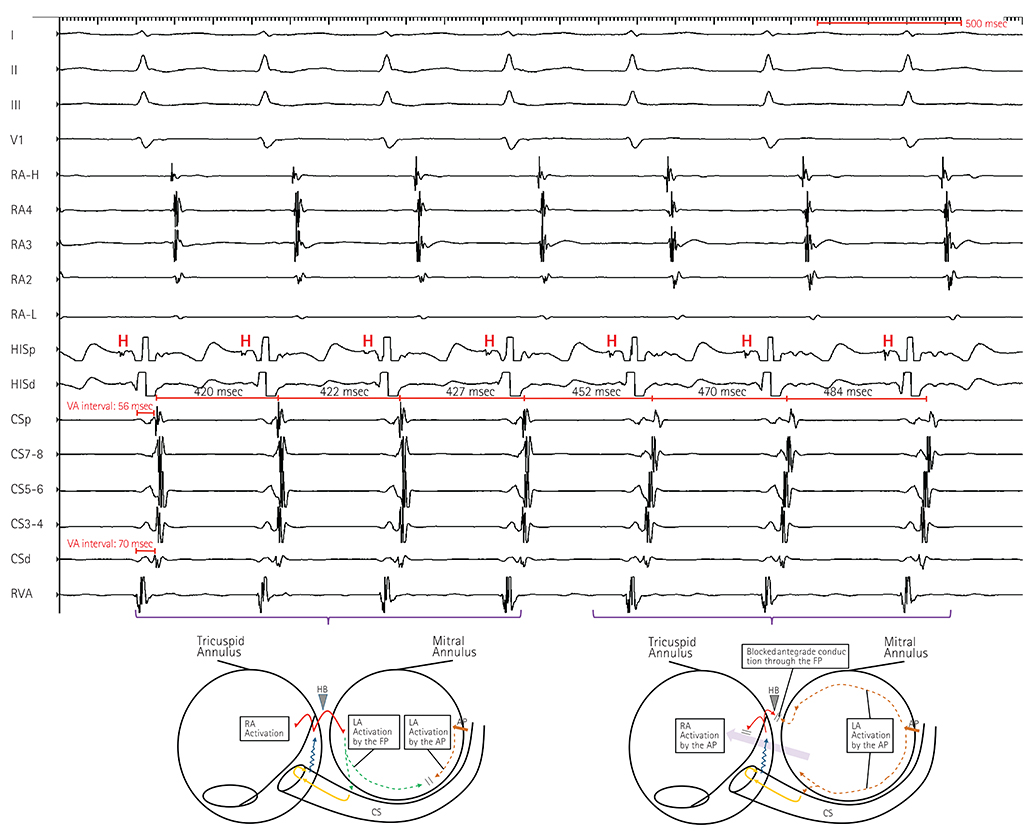
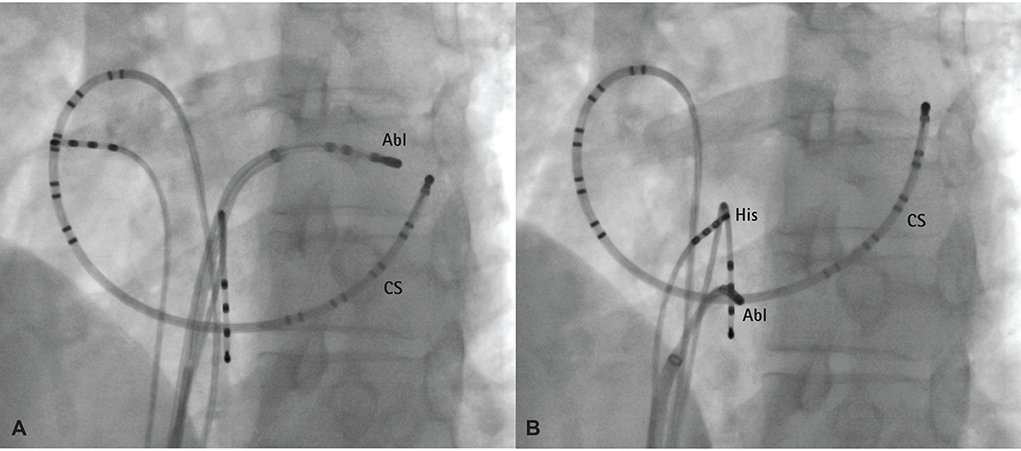
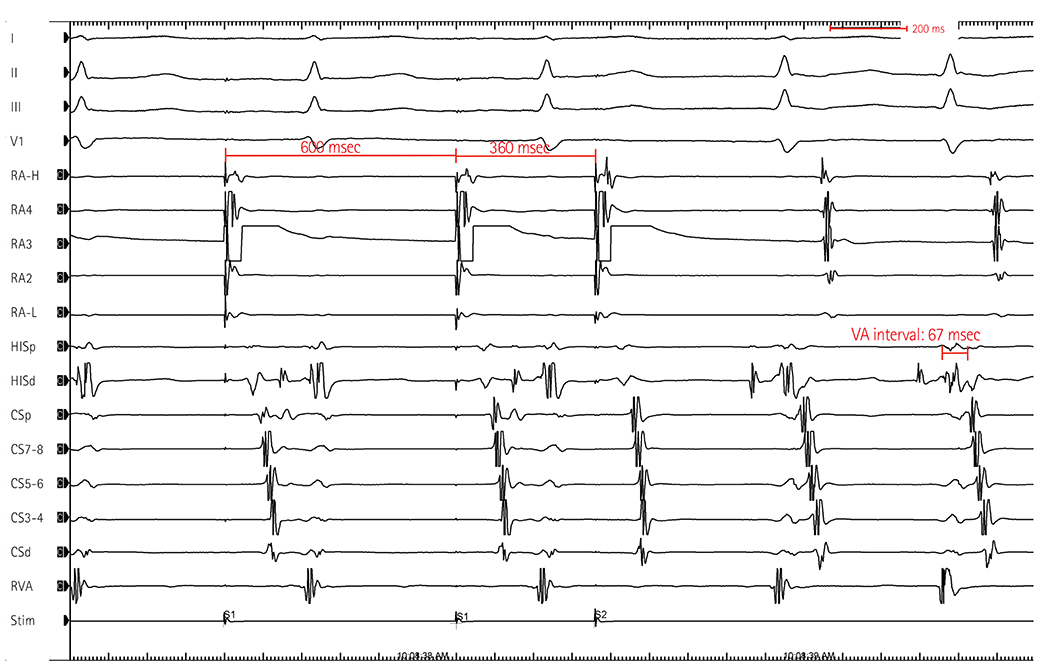
- Among patients with Wolff-Parkinson-White syndrome, atrioventricular reciprocating tachycardia (AVRT) and atrioventricular nodal reentrant tachycardia (AVNRT) can coexist in a single patient. Direct transition of both tachycardias is rare; however, it can occur after premature atrial or ventricular activity if the cycle lengths of the two tachycardias are similar. Furthermore, persistent atrial activation by an accessory pathway (AP) located outside of the AV node during ongoing AVNRT is also rare. This article describes a case of uncommon atrial activation by an AP during AVNRT and gradual transition of the two supraventricular tachycardias without any preceding atrial or ventricular activity in a patient with preexcitation syndrome.
Keyword
MeSH Terms
Figure
Reference
-
1. Gallagher JJ, Pritchett EL, Sealy WC, Kasell J, Wallace AG. The preexcitation syndromes. Prog Cardiovasc Dis. 1978; 20:285–327.2. Delacretaz E, Soejima K, Stevenson WG, Friedman PL. Short ventriculoatrial intervals during orthodromic atrioventricular reciprocating tachycardia: what is the mechanism? J Cardiovasc Electrophysiol. 2000; 11:121–124.3. Rakovec P. Transition of orthodromic tachycardia into atrioventricular nodal tachycardia during radiofrequency ablation of an accessory pathway. Europace. 2009; 11:1563–1565.4. Kuo JY, Tai CT, Chiang CE, et al. Mechanisms of transition between double paroxysmal supraventricular tachycardias. J Cardiovasc Electrophysiol. 2001; 12:1339–1345.5. Crawford TC, Mukerji S, Good E, et al. Utility of atrial and ventricular cycle length variability in determining the mechanism of paroxysmal supraventricular tachycardia. J Cardiovasc Electrophysiol. 2007; 18:698–703.6. Hwang C, Martin DJ, Goodman JS, et al. Atypical atrioventricular node reciprocating tachycardia masquerading as tachycardia using a left-sided accessory pathway. J Am Coll Cardiol. 1997; 30:218–225.7. Tada H, Naito S, Taniguchi K, Nogami A. Concealed left anterior accessory pathways: two approaches for successful ablation. J Cardiovasc Electrophysiol. 2003; 14:204–208.8. Luria DM, Nemec J, Etheridge SP, et al. Intra-atrial conduction block along the mitral valve annulus during accessory pathway ablation: evidence for a left atrial "isthmus". J Cardiovasc Electrophysiol. 2001; 12:744–749.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atrial fibrillation in patient with Wolff-Parkinson-White syndrome mimicking ventricular tachycardia
- One Case of Cerebral Embolism Associated with Paroxysmal Tachycardia in Wolff-Parkinson-White Syndrome
- Two Cases of Wolff-Parkinson-White Syndrome in a Family
- Wolff-Parkinson-White Syndrome Treated with Radiofrequency Ablation in Father and His Son
- A Case of Early Onset MELAS Patient with Wolff-Parkinson-White Syndrome