J Korean Med Assoc.
2011 Jul;54(7):715-724.
Orthopedic disease and sports medicine related to lower limbs
- Affiliations
-
- 1Department of Orthopaedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Physical Medicine and Rehabilitation, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wonhah.park@samsung.com
Abstract
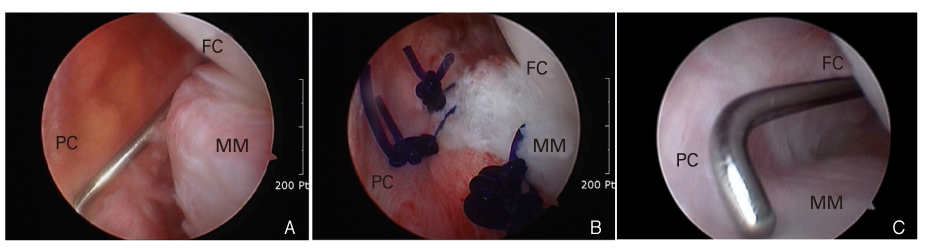
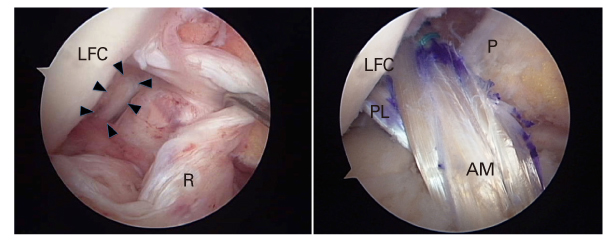
- In this study, the cause, diagnosis, and treatment of common lower limb injuries during the sports activities were presented. Sports injuries of the lower limbs are the most common injuries in the sports medicine field due to the high level of use of the lower limbs during sports activities. The common causes of leg injuries in athletes are traumatic force over the critical limit of normal tissue, repetitive microtrauma, and overuse. Common hip and pelvis problems encountered by the authors include trochanteric bursitis, snapping hip syndrome, and labral tears. The anterior and posterior cruciate ligaments, medial and lateral collateral ligaments, and meniscus have been most frequently involved in sports injuries affecting the knees. Lateral ankle sprain represents one of common injuries in the athletic population. Common overuse injuries are tendinopathies, stress fractures, chronic exertional compartment syndrome, and shin splints. Athletic activity provides a variety of positive benefits to participants' health. To safely continue those activities, an injury prevention program focusing on injuries that may occur in specific sports activities is recommended for participants. Early diagnosis and proper treatment are also important in promoting prompt recovery and preventing secondary injuries.
Keyword
MeSH Terms
-
Animals
Ankle
Athletes
Athletic Injuries
Bursitis
Collateral Ligaments
Compartment Syndromes
Cumulative Trauma Disorders
Early Diagnosis
Femur
Fractures, Stress
Hip
Humans
Knee
Leg Injuries
Lower Extremity
Medial Tibial Stress Syndrome
Orthopedics
Pelvis
Posterior Cruciate Ligament
Sports
Sports Medicine
Sprains and Strains
Tendinopathy
Figure
Reference
-
1. Slawski DP, Howard RF. Surgical management of refractory trochanteric bursitis. Am J Sports Med. 1997. 25:86–89.
Article2. McCarthy JC, Busconi B. The role of hip arthroscopy in the diagnosis and treatment of hip disease. Orthopedics. 1995. 18:753–756.
Article3. Ilizaliturri VM Jr, Villalobos FE Jr, Chaidez PA, Valero FS, Aguilera JM. Internal snapping hip syndrome: treatment by endoscopic release of the iliopsoas tendon. Arthroscopy. 2005. 21:1375–1380.
Article4. Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006. 186:449–453.
Article5. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005. 21:1496–1504.
Article6. Akseki D, Ozcan O, Boya H, Pinar H. A new weight-bearing meniscal test and a comparison with McMurray's test and joint line tenderness. Arthroscopy. 2004. 20:951–958.
Article7. Muellner T, Weinstabl R, Schabus R, Vécsei V, Kainberger F. The diagnosis of meniscal tears in athletes. A comparison of clinical and magnetic resonance imaging investigations. Am J Sports Med. 1997. 25:7–12.8. Jacobson KE, Chi FS. Evaluation and treatment of medial collateral ligament and medial-sided injuries of the knee. Sports Med Arthrosc. 2006. 14:58–66.
Article9. Beynnon BD, Fleming BC. Anterior cruciate ligament strain in-vivo: a review of previous work. J Biomech. 1998. 31:519–525.
Article10. Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976. 4:84–93.
Article11. Drogset JO, Grøntvedt T, Robak OR, Mølster A, Viset AT, Engebretsen L. A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 2006. 88:944–952.
Article12. Van Dommelen BA, Fowler PJ. Anatomy of the posterior cruciate ligament. A review. Am J Sports Med. 1989. 17:24–29.13. Covey CD, Sapega AA. Injuries of the posterior cruciate ligament. J Bone Joint Surg Am. 1993. 75:1376–1386.
Article14. Esmaili Jah AA, Keyhani S, Zarei R, Moghaddam AK. Accuracy of MRI in comparison with clinical and arthroscopic findings in ligamentous and meniscal injuries of the knee. Acta Orthop Belg. 2005. 71:189–196.15. Shelbourne KD, Muthukaruppan Y. Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy. 2005. 21:457–461.
Article16. Cooper JM, McAndrews PT, LaPrade RF. Posterolateral corner injuries of the knee: anatomy, diagnosis, and treatment. Sports Med Arthrosc. 2006. 14:213–220.
Article17. Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy. 1996. 12:521–530.
Article18. Thacker SB, Stroup DF, Branche CM, Gilchrist J, Goodman RA, Weitman EA. The prevention of ankle sprains in sports. A systematic review of the literature. Am J Sports Med. 1999. 27:753–760.19. Aktas S, Kocaoglu B, Nalbantoglu U, Seyhan M, Guven O. End-to-end versus augmented repair in the treatment of acute Achilles tendon ruptures. J Foot Ankle Surg. 2007. 46:336–340.
Article20. Maffulli N, Khan KM, Puddu G. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy. 1998. 14:840–843.
Article21. Davies SG, Baudouin CJ, King JB, Perry JD. Ultrasound, computed tomography and magnetic resonance imaging in patellar tendinitis. Clin Radiol. 1991. 43:52–56.
Article22. Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med. 2000. 29:135–146.23. Huang HH, Qureshi AA, Biundo JJ Jr. Sports and other soft tissue injuries, tendinitis, bursitis, and occupation-related syndromes. Curr Opin Rheumatol. 2000. 12:150–154.
Article24. Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987. 15:46–58.25. Opstad PK, Aakvaag A. Decreased serum levels of oestradiol, testosterone and prolactin during prolonged physical strain and sleep deprivation, and the influence of a high calorie diet. Eur J Appl Physiol Occup Physiol. 1982. 49:343–348.
Article26. Rupani HD, Holder LE, Espinola DA, Engin SI. Three-phase radionuclide bone imaging in sports medicine. Radiology. 1985. 156:187–196.
Article27. Micheli LJ, Solomon R, Solomon J, Plasschaert VF, Mitchell R. Surgical treatment for chronic lower-leg compartment syndrome in young female athletes. Am J Sports Med. 1999. 27:197–201.
Article28. Edwards P, Myerson MS. Exertional compartment syndrome of the leg: steps for expedient return to activity. Phys Sportsmed. 1996. 24:31–46.29. Andrish JT, Bergfeld JA, Walheim J. A prospective study on the management of shin splints. J Bone Joint Surg Am. 1974. 56:1697–1700.
Article30. Michael RH, Holder LE. The soleus syndrome. A cause of medial tibial stress (shin splints). Am J Sports Med. 1985. 13:87–94.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Analysis of Upper Limbs Injury Types of Snowboarding in 2004-2008 Season
- Acute Cervical Myelopathy Due to Ruptured Disc During Leisure Sports Activity in Adjacent Segment
- Norm-Referenced Criteria for Isokinetic Strength of the Lower Limbs for the Korean High School Baseball Players
- Vaccination for Athletes: Evidence and Recommendations
- Ultrasonography for Diagnosing Sports-Related Shoulder Pain