J Korean Ophthalmol Soc.
2014 Aug;55(8):1180-1186.
The Long-Term Outcome of Lateral Rectus Advancement in Patients with Consecutive Esotropia Following Bilateral Lateral Rectus Recession for Intermittent Exotropia
- Affiliations
-
- 1Department of Ophthalmology, Gachon University Gil Medical Center, Incheon, Korea. hjpaik@gilhospital.com
Abstract
- PURPOSE
To investigate the long-term outcome of lateral rectus (LR) advancement for consecutive esotropia following bilateral LR recession for intermittent exotropia.
METHODS
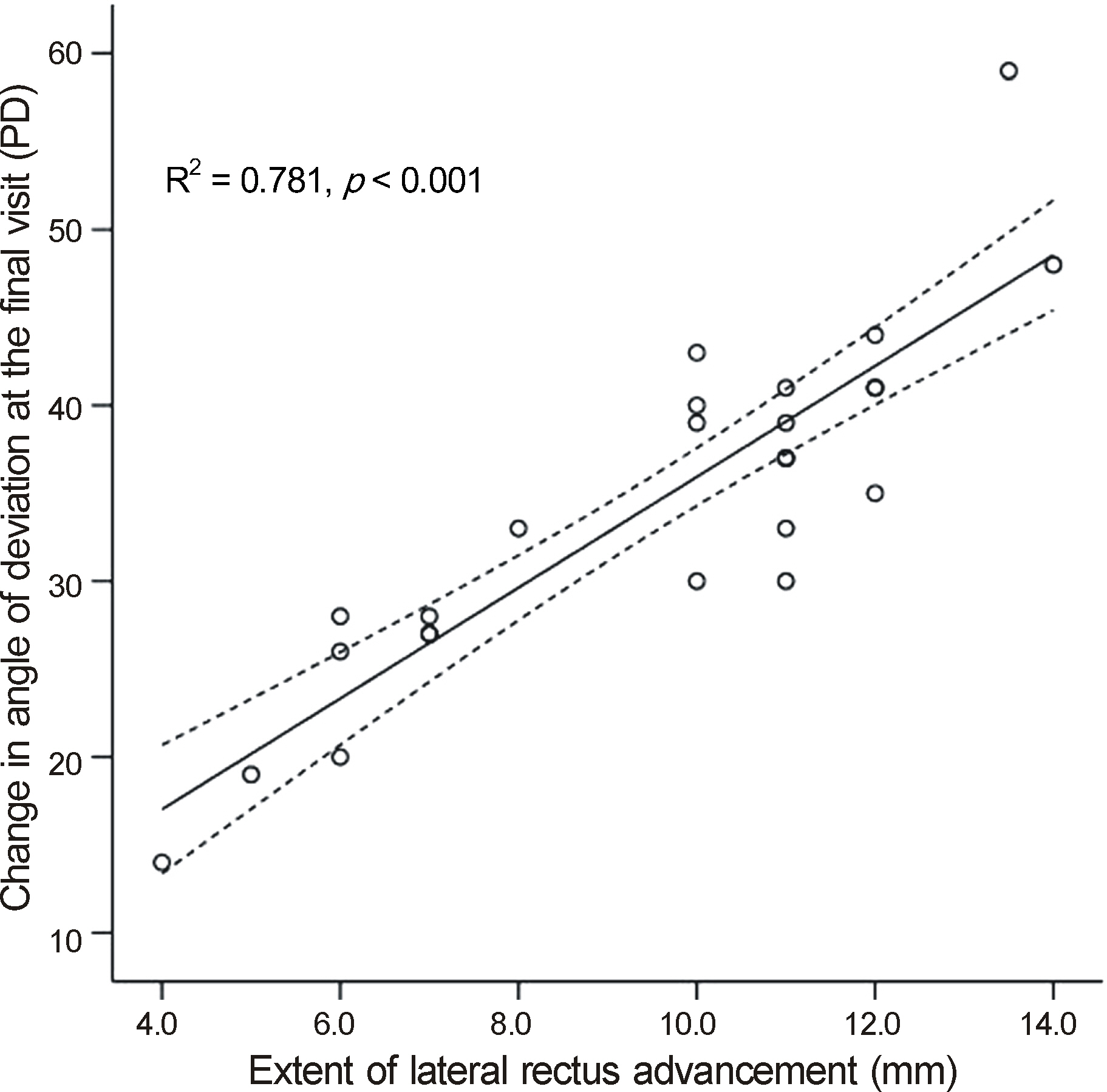
Medical records of 25 patients who underwent LR advancement for consecutive esotropia after bilateral LR recession and who were followed up for more than 24 months postoperatively were reviewed. Patients were divided into two groups: bilateral lateral rectus recession (BLR) group included 16 patients with consecutive esotropia greater than or the same magnitude as the initial exotropia and who underwent bilateral LR advancement; Unilateral lateral rectus recession (ULR) group included nine patients with consecutive esotropia less than the initial exotropia and who underwent unilateral LR advancement. Main outcome measurements were motor and sensory outcomes and the dose-effect relationship calculated from observed overall and group changes in the angle of deviation per millimeter. Motor success was defined as alignment from orthotropia to exodeviation less than 10 PD at distance. Sensory outcome was described by comparing the Titmus stereoacuity test before and after LR advancement. Sensory successvwas defined at 100 seconds of arc.
RESULTS
Eighteen patients (72.0%) showed satisfactory long-term motor and sensory outcomes. Seventeen (77.3%) of 22 patients showed favorable stereopsis of 100 seconds of arc or more at final observation. The long-term motor success rate of the ULR group was better than that of the BLR group (p = 0.025). The average observed change in the angle of deviation was 3.6 PD/mm at the final visit in all patients. A greater dose-effect relationship was observed in the ULR group than in the BLR group at the final visit (p = 0.043).
CONCLUSIONS
LR advancement showed favorable motor and sensory outcomes in the majority of patients. The surgical outcome was not favorable in patients in the BLR group with consecutive esotropia of the same magnitude as the initial exotropia. These results require further investigation for verification.
Figure
Reference
-
References
1. Raab EL, Parks MM. Recession of the lateral recti. Early and late postoperative alignments. Arch Ophthalmol. 1969; 82:203–8.2. Scott WE, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol. 1981; 99:1814–8.
Article3. Ruttum MS. Initial versus subsequent postoperative motor alignment in intermittent exotropia. J AAPOS. 1997; 1:88–91.
Article4. Maruo T, Kubota N, Sakaue T, Usui C. Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment. A study of 666 cases. Binocul Vis Strabismus Q. 2001; 16:265–70.5. Lee S, Lee YC. Relationship between motor alignment at postoperative day 1 and at year 1 after symmetric and asymmetric surgery in intermittent exotropia. Jpn J Ophthalmol. 2001; 45:167–71.
Article6. Kim TW, Kim JH, Hwang JM. Long-term outcome of patients with large overcorrection following surgery for exotropia. Ophthalmologica. 2005; 219:237–42.
Article7. Hardesty HH. Treatment of overcorrected intermittent exotropia. Am J Ophthalmol. 1968; 66:80–6.
Article8. Edelman PM, Murphree AL, Brown MH, Wright KW. Consecutive esodeviation…then what. Am Orthopt J. 1988; 38:111–6.9. Park SH, Kim HK, Jung YH, Shin SY. Unilateral lateral rectus advancement with medial rectus recession vs bilateral medial rectus recession for consecutive esotropia. Graefes Arch Clin Exp Ophthalmol. 2013; 251:1399–403.
Article10. Cooper EL. The surgical management of secondary exotropia. Trans Am Acad Ophthalmol Otolaryngol. 1961; 65:595–608.11. Lee JH, Lee SY, Lee YC. The effect of lateral rectus muscle advancement in consecutive esotropia after bilateral rectus muscle recession. J Korean Ophthalmol Soc. 2008; 49:1801–6.
Article12. Kim JS, Son KH. The effect of advancement of the lateral rectus muscle on the consecutive esotropia. J Korean Opthalmol Soc. 1995; 36:1784–9.13. Lee EK, Hwang JM. Prismatic correction of consecutive esotropia in children after a unilateral recession and resection procedure. Ophthalmology. 2013; 120:504–11.
Article14. Jang JH, Park JM, Lee SJ. Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefes Arch Clin Exp Ophthalmol. 2012; 250:1485–90.
Article15. Cho YA, Ryu WY. The advancement of the medial rectus muscle for consecutive exotropia. Can J Ophthalmol. 2013; 48:300–6.
Article16. Ohtsuki H, Hasebe S, Tadokoro Y, et al. Advancement of medial rectus muscle to the original insertion for consecutive exotropia. J Pediatr Ophthalmol Strabismus. 1993; 30:301–5.
Article17. Biedner B, Yassur Y, David R. Advancement and reinsertion of one medial rectus muscle as treatment for surgically overcorrected esotropia. Binocul Vis Strabismus Q. 1991; 6:197–200.18. Kasi SK, Tamhankar MA, Pistilli M, Volpe NJ. Effectiveness of medial rectus advancement alone or in combination with resection or lateral rectus recession in the management of consecutive exotropia. J AAPOS. 2013; 17:465–70.
Article19. Chatzistefanou KI, Droutsas KD, Chimonidou E. Reversal of unilateral medial rectus recession and lateral rectus resection for the correction of consecutive exotropia. Br J Ophthalmol. 2009; 93:742–6.
Article20. Mohan K, Sharma A, Pandav SS. Unilateral lateral rectus muscle recession and medial rectus resection with or without advancement for postoperative consecutive exotropia. J AAPOS. 2006; 10:220–4.21. Patel AS, Simon JW, Lininger LL. Bilteral lateral rectus recession for consecutive exotropia. J AAPOS. 2000; 4:291–4.22. Smith KA, Nischal KK. Consecutive exotropia: does one size fit all. Br J Ophthalmol. 2009; 93:706–7.
Article23. Yang HK, Hwang JM. Bilateral vs unilateral medial rectus resection for recurrent exotropia after bilateral lateral rectus recession. Am J Ophthalmol. 2009; 148:459–65.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Advancement of the Lateral Rectus Muscle on the Consecutive Esotropia
- Clinical Evaluation on the Consecutive Esotropia after Exotropia Surgery
- Consecutive Esotropia after Surgical Correction of Intermittent Exotropia
- The Effect of Lateral Rectus Muscle Advancement in Consecutive Esotropia After Bilateral Rectus Muscle Recession
- Unilateral Lateral Rectus Muscle Advancement Surgery Based on One-fourth of the Angle of Consecutive Esotropia